A Four Month Detour…
Posted on December 24, 2025
I really didn’t mean to abandon this blog but the last four months have been completely miserable, healthwise.
Less than a week after I last posted, I started experiencing what felt like electric shocks in my lower back. It was so painful that, at times, all I could do was scream. Even when the electric-shock-like spasms weren’t actively happening, I was in – quite possibly – the worst pain I’ve ever experienced. And given my experience with chronic pain, that’s saying something. It was horrendous, especially as the painkillers that usually give me some relief weren’t having any effect. Eventually I managed to get some stronger painkillers from my GP and they were so strong that, for the first few days, I could barely keep my eyes open: I was asleep for around twenty hours each day. Thankfully, that did wear off after a while but I still felt slow and blurry while taking them.
It was a completely new kind of pain for me and while we had a few theories from the network of health professionals I’ve worked with, we still didn’t know what was causing it, how long it would go on for, or if it was a permanent change. The massage therapist I’ve done some work with – who has both personal and professional experience of Hypermobile Ehlers-Danlos Syndrome and chronic pain – was a godsend and thankfully, my Mum found a new physiotherapist nearby who had professional experience with hEDS and who was able to come to the house to see me. He was fantastic: he was thoughtful and thorough and explained everything with great care (sometimes multiple times); he really listened to me and took my priorities into account when choosing the exercises for me to do; I felt like he actually cared about me as a whole person, which has not been a common experience. He assessed me and felt that I had a pinched nerve in my lumbar spine, which typically heals in about eight to twelve weeks. That felt like an interminably long time but I was relieved to hear that he expected the pain to go away. He gave me some very gentle exercises to do as I felt able to, with the goal of strengthening the muscles in my back to support my especially hypermobile lumbar spine (and hopefully reduce my chronic pain). Between the pills (despite the side effects), the massage, the physiotherapy exercises, and the time that I was forced to take to rest properly, the pain finally started to decrease and I was able to slowly increase my mobility – I’m still working on that.
Unfortunately that was only the first part of the story. In early October, I started to struggle with multiple symptoms that I’ve rarely experienced, including stomach pain, nausea, acid reflux, and difficulty swallowing. It made eating so difficult that I could barely keep any food down and it made sleeping difficult because I felt worse when I was lying down. I felt awful but my Mum had been unwell a week or so earlier and so I assumed that it was the same thing and would pass relatively quickly; I thought I just had to rest and wait it out, like I often do with a seasonal illness or the symptoms of my chronic illnesses. But that didn’t happen. The symptoms got more intense until I wasn’t eating at all – sips of water were all I could manage – and the POTS symptoms I experience everyday had become debilitating. I hate going to the doctor but if there was ever a time, this was it.
I managed to get an appointment with one of the GPs pretty quickly – not my usual GP but that isn’t unusual and I did manage to get an appointment with her for later in the week – but when I explained what was happening, this doctor said that there wasn’t time to explore each of the symptoms so she questioned me about the difficulty swallowing, prescribed me a medication, and sent me on my way. I was deeply unimpressed and had no confidence in her diagnosis or the medication: treating one symptom when several are presenting at the same time… that seemed very unlikely to help whatever was causing the multiple symptoms. I’m passionate about the NHS (and about improving it) but it’s not exactly straightforward when I’ve been repeatedly invalidated and mistreated by medical professionals.
I didn’t have time to even take the medication before the stomach pain got so bad that I couldn’t move. We ended up calling 111 and their recommendation was to call an ambulance and head to A&E. The idea of being in an ambulance – as an already overstimulated autistic person – felt horrific and I almost had a meltdown; I didn’t know what I was supposed to do when I felt like I could barely move. Eventually my Mum had to all but drag me into a cab to go to A&E. For once, being autistic was a help rather than a hindrance because the receptionist moved us straight from the initial waiting room into the actual A&E department where people were being assessed and treated. We still had a considerable wait ahead of us, which felt incredibly long given how much pain I was in. It wasn’t exactly a restful environment either: besides the patients and nurses coming in and out, there were paramedics and police and one young woman who cried the entire time she was there. If I hadn’t been in so much pain and so overstimulated, I might’ve been impressed – and a lot more sympathetic. But I was running on empty and on the edge of sensory overload and all I wanted was some quiet; it was a rough night – for everyone clearly.
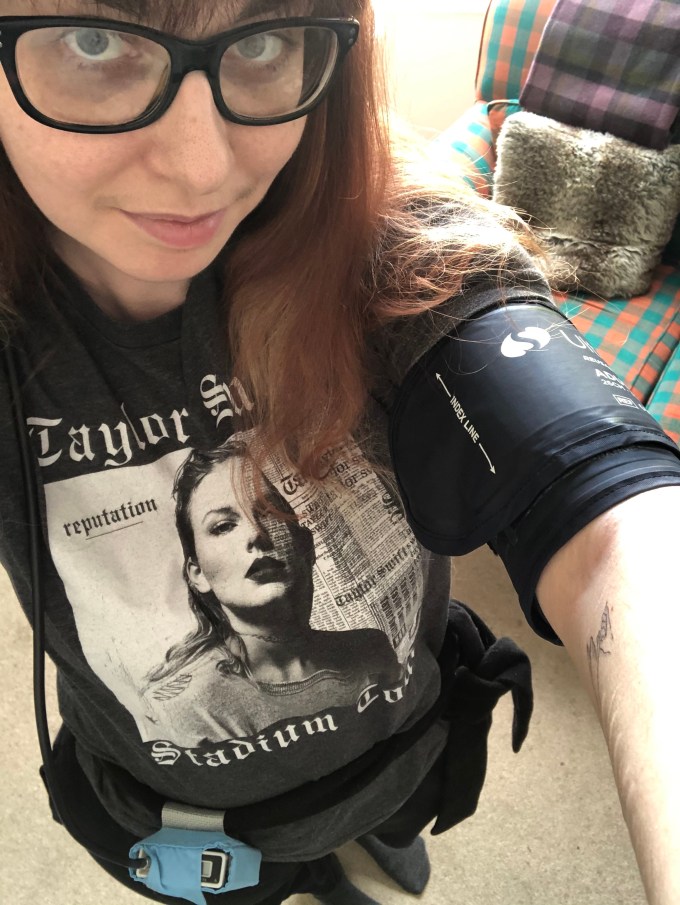
After a couple of hours, several different nurses did a series of tests, including taking blood and doing an ECG (during which my cannula from the blood draw was jostled, leading to the bruise pictured below – that hurt for a while). A little while later, another nurse gave me a low dose of morphine that did, thankfully, slowly bring my pain level down. But after that, we were left for several hours; even when we were the only people left in the little waiting area, no one came for us or even gave us an update. I was starting to think we’d been forgotten about.
When a doctor did finally call my name, he didn’t have any real answers for me. He did at least have a reasonable understanding of hEDS and how it can cause strange or skewed test results: a hEDS body does not react to anything the same way a non-hEDS body does, surprise surprise. So there was no obvious explanation for my symptoms but he prescribed antibiotics and recommended getting a referral to the hospital’s Gastroenterology department if the symptoms weren’t resolved by the antibiotics. I don’t love the approach of just throwing medication at a problem and hoping it helps but I was desperate and that was the only option being offered.


(Left: the bruise left by my cannula, having being knocked during A&E tests // Right: me, asleep on the sofa the day after the night spent in A&E with Izzy keeping me company)
We got home around seven and I was asleep the moment I lay down on the sofa. I was just completely exhausted. I took the antibiotics I’d been prescribed but then, when I saw my actual GP, she was surprised by how high the dose was, adjusted it, and prescribed another antibiotic, as well as sending the referral to the Gastroenterology department at the hospital. Again, it wasn’t exactly reassuring since we still didn’t know what the actual problem was and I was starting to spiral a bit about the possibility that this was more than just a passing illness, that it was something much more serious that was getting overlooked (with the potential to lead to an even more debilitating outcome). But I tried not to go down that rabbit hole. I was trying to at least give the various medications a chance to work.
Over the next few weeks, I just lay on the sofa and tried to eat when I felt able to. Between my body trying to fight whatever was going on and the fact that it was trying to function on very little fuel, I was barely able to do anything. I was forced to rest, to literally just rest; I couldn’t even do the most passive of activities. I was physically, mentally, and emotionally exhausted. My body and my brain were barely functioning: a good day consisted of a shower and watching TV (and eating what I could). But the medications started to work and, very slowly, I started to feel better and the symptoms started to decrease in intensity, even if I was still building back up my capacity after so long with so little fuel in my body. And then, just as I was finishing the courses of medication, I started to feel actually well again and I don’t think describing my mood as “overjoyed” would be an exaggeration. Eating went from being a struggle to being joyful (a word I don’t think I’ve ever used in the context of eating) and I was sleeping well, not only for the first time in weeks but in months: I was feeling so good that it felt more than a little surreal but I wasn’t complaining. It was a huge relief after eight weeks of feeling so terrible.
But less than a week later, the symptoms started to reappear and I started to feel really unwell again. I had bloodwork done (which had been ordered way back when I’d first gone to the doctor) but all of the tests came back fine or inconclusive again. I was wondering if the medications had been treating just the symptoms and not the underlying issue, which made me deeply anxious about what that underlying issue could be. I wasn’t sure what the next step was supposed to be but I’ve had a lot of conversations with a lot of different people in my various circles and, long story short, it seems that these digestive issues were a delayed response to the increase of one of my long term medications: some (professionally guided) experimentation has proved as much as is possible that my digestive system can’t handle this medication over a certain dosage so I’m currently taking a break from it (which is something you can safely do with this medication) while getting my food routine and some of my energy and strength back. After Christmas, or maybe the New Year, we’ll reassess and I’ll likely start taking it again at the lower dose since I had had a positive experience with it until that final dosage increase.
So that is where I’ve been: too sick to do anything, too sick to even write a blog post about being sick. When I say it’s the most unwell I’ve ever felt, I’m not exaggerating. I’ve dealt with a wide range of symptoms and various levels of pain during my life but never have I been so ill, in the way we typically picture illness. I’ve dialled everything right back to absolute basics and I am starting to feel a bit more normal, despite a few bumps in the road. Fingers crossed, I’ll be feeling more like myself again by the time the New Year rolls around…
Category: animals, autism, blog, chronic fatigue, chronic pain, food, heds, medication, pots, sleep, treatment Tagged: a&e, accident and emergency, acid reflux, antibiotics, anxiety, asd, autism, autism spectrum disorder, autistic blogger, back pain, blood tests, chronic illness, chronic pain, chronically ill, eds, ehlers danlos syndrome, heds, hospital referral, hypermobile ehlers danlos syndrome, ill, illness, medical anxiety, medical trauma, medication, medication intolerance, medication side effects, nausea, nhs, pain medication, physiotherapy, pinched nerve, postural orthostatic tachycardia syndrome, pots, recovery, rest, sick, sickness
Migraines, Tooth Pain, And Blood Pressure Monitoring
Posted on June 5, 2021
So often in my life it seems, medical stuff is like waiting for a bus: weeks or months go by and then suddenly a whole slew of them show up. And that’s certainly been true of the last few months. Just as the final module of my Masters was starting, I was hit by a series of awful migraines, suffered with terrible tooth pain, and spent twenty four hours hooked up to a blood pressure monitor, a test ordered by a neurology unit in London. So it’s been a pretty hectic time…
MIGRAINES
At the time of writing this, I’ve lost approximately half of the last forty days to migraines.
I’ve had migraines before – maybe a handful a year, depending on my stress levels and the medication I’m taking – but they usually only last for a day or so before fading away. They’re not pleasant but they weren’t seriously impacting my life. But then I had one that lasted roughly four days and I ended up in A&E because, having fairly recently had the Astra Zeneca vaccine, my doctor was worried about the extremely rare side effect of a blood clot. I was sure it was a migraine but agreed to go and after most of the day there, I was released; the doctor agreed that it was most likely a bad migraine but told me to come back if it didn’t go away. And after another day or so, it did. While I was somewhat irritated about losing a day that should’ve been spent working on my end of semester assessment (despite the pain, I was pushing myself to work on it as I could, in the moments where the painkillers actually worked – I think that’s mainly why it went on so long personally), I am really grateful to all of the hospital staff. They were all great – warm, considerate, and personable – despite the somewhat alarming COVID precautions everywhere that weren’t exactly great for my anxiety. But they were really kind and gentle with me throughout my visit, making the whole experience a lot easier than it could’ve been.
I’d thought that that was it. But then, again and again, I was hit by migraine after migraine, all lasting unusually long periods of time (for me, at least). They were averaging out at about six days each time, sometimes more. That was extremely stressful, bearing in mind that I’m at the beginning of the homestretch of my Masters with this final module accounting for 60% of my final grade, and I was utterly miserable from the pain. I was also so light sensitive; at one point, even the darkest room in the house felt too bright and I dissolved onto the floor in tears, which only hurt my head more. It was awful. That was the first time we called 111 and they called paramedics. That time they determined it was, again, a severe migraine and recommended two other pain medications to try in the hope that they’d be more effective than Nurofen.
A couple of migraines later, with minimal help from the new painkillers, I had another really bad one, which had us calling 111 and they sent paramedics (both such lovely guys who fell in love with the cats and talked musicals with me while they did their tests). This migraine was slightly different: it had all of my normal migraine symptoms but I also had this almost blinding pain at the front and right side of my face. They thought it was probably a migraine but suggested talking to my doctor about having a CAT scan and/or whether there was something going on with my cranial nerves. They also had some practical, experience based advice around pain relief (one of them had personal experience with severe migraines). They said they could escort us to the hospital on the off chance that a doctor would do a CAT scan but did acknowledge that they might just take blood and keep me there while it was checked again, like my previous visit to A&E. So we chose the second option: Mum was going to go out and get the new medication option and call my GP ASAP.
TOOTH PAIN
That was the most recent migraine (at the time of writing this). As time passed, the pain in my head started to decrease, then my face, settling in my back-top-right teeth; every time they – and finally just one (after about a week) – knocked against the bottom teeth, the pain was so bad that my entire body would freeze up.
As soon as it had settled in my teeth, we’d called the dentist and they brought me in as an emergency (a few days wait rather than a few months). The dentist checked, took x-rays and saw some decay in the painful tooth, fairly close to the nerve root, and it already has a pretty big filling in it. At one point, somehow, the hEDS diagnosis came up (I was diagnosed since my last dental appointment) and the dentist said that she’s seen and heard about multiple people with a form of EDS (or who were later diagnosed with it) struggle with tooth decay, as well as being scolded by their dentists for not doing a good enough job with their dental hygiene even though they actually were; it was often the EDS causing problems, not necessarily their actions. This really is the diagnosis that keeps on giving (imagine a sarcastic snort at the end of that sentence).
Anyway, she diagnosed an abscess and gave me two treatment options: extraction or root canal therapy, which would involve multiple, multi-hour sessions that would be painful, ultimately might not work, and probably wouldn’t last into my late thirties. The whole thing felt pretty overwhelming and I ended up in tears. Extraction was the obvious choice as far as I was concerned and everyone else agreed; there seemed to be way too many downsides to the root canal option (plus it sounded horrendous and I find dental work, even fairly straightforward stuff, very distressing) and even if I was inclined to choose it, it’s the worst possible time given the end of my Masters. Even an extraction is going to be a significant disruption. I’m applying for extenuating circumstances, which both my supervisor and module leader have encouraged, so hopefully that’ll mean I end up with the same amount of time to do the work as everyone else.
So, I’ve been referred for an emergent extraction under general anaesthetic but I don’t know when that’s going to happen. They also prescribed me some antibiotics for the mean time. Now it’s a waiting game. But several days after the appointment, either the antibiotics are working or the nerve is dying or both because the pain is getting better and I feel more human. There are periods of time where I can actually ignore it, which is a huge deal considering how much pain I’d been in. So that’s definitely something to be grateful for.
BLOOD PRESSURE MONITORING
A couple of months ago, I had an appointment with a doctor from a neurology unit in London, which I believe I mentioned in this post. After spending most of the appointment vehemently telling me there was no point in getting any tests, he somewhat reluctantly offered to write to my GP, suggesting I have my blood pressure monitored for twenty four hours. It took forever to get a monitor from the hospital but finally test day came.
I had to go to the hospital where they fitted the monitor (found the right size for my arm, wrapped me up, made sure it was taking readings, looped the cable behind my neck, and used the tie from my coat to secure the monitor/data recorder around my waist) and gave me the instructions and paperwork to go along with the monitor. I wasn’t allowed to get it wet so I couldn’t have a shower while wearing it but since that’s when I usually get my blood pressure related symptoms, we devised a plan where I would go through the motions – with the shower on to create the heat and steam – so that it would still record whatever was happening to my blood pressure during a shower, as much as possible at least. The whole process was relatively stress free and the two women who sorted me out were great, warm and extremely competent but flexible to my needs. I’m really grateful to them for making it so easy.
All done, we headed home. It was a bit weird with the weight of the monitor, the too long cable getting caught on stuff, and so on but overall, it was fine. The cuff got very tight – tighter than I remembered them getting when you get a one off test – but it wasn’t a big deal and the rest of the day went on as normal. It was a bit of a struggle to get to sleep because I couldn’t get comfortable with the cuff on my arm but once I did get to sleep, the inflating and squeezing didn’t wake me up, something I’d expected to happen.
However, when I woke up, my arm was really sore. I felt like I’d been punched a hundred times in the same place, convinced the skin was bruised underneath the cuff (it wasn’t and no bruise ever emerged but damn, it was tender). I think the cuff had slipped in the night as well because I had several error readings on that second day.
I had my pretend shower and, as usual, felt shaky, dizzy, and lightheaded; having thought ahead, I’d timed things so that the monitor would be taking the reading right at the end of my fake shower. I’m intrigued to see what that reading says. That done, Mum helped me wash my hair, leant over the side of the bath; I had an online meeting and couldn’t bear the thought of doing that with unwashed hair. It wasn’t very dignified, especially with all the extra towels wrapped around me to keep the monitor dry, but it got the job done.
I wore it for the rest of the twenty four hours and then, with great relief, unwrapped the cuff. By the end, my arm felt really sore from the squeezing, plus it had started to pinch in various places at some point. There’s also that Autism-sensory-thing of wearing something constantly constricting, which starts causing anxiety after certain periods of time, like a long day in skinny jeans or wearing my retainer all day. Does that make sense? The anxiety had been building for the last few hours and it was wonderful to take it off.
Mum dropped it back at the hospital, so now I guess it’s another waiting game. I don’t know when we’ll find out the results and the conclusions drawn from them. I assume that they’ll let us know at some point, although it wouldn’t be the first time we’ve had to chase results. As I said, all we can do now is wait.
So, yeah, hectic. At a very inconvenient time. But that’s life and I’m determined not to let it spoil the last of my Masters and this project that I’ve been looking forward to for so long. I am going to make the most of every good day I have, take the extenuating circumstances gratefully, and continue working as hard as I can.
Category: diagnosis, event, medication, treatment, university Tagged: a&e, blood pressure, blood pressure monitoring, dentist, health, hospital, masters degree, masters degree year two, masters part time, migraine, migraines, pain, paramedics, physical health, physical pain, student, tooth pain, university
What I Did In Lockdown – Part 3
Posted on April 24, 2021
So, on the 4th January, England went into another national lockdown and this list was once again revived. This one felt much more like the first lockdown than the second, where many schools, businesses, etc were still open. When schools and universities started to open, my course remained online (it was one of the courses that could function solely online and meant less people going back to the uni) so lockdown continued for me. My life has only just started to involve going out again – swimming, getting a haircut, (safely) seeing a few people – and that’s why I’ve kept this list going as long as I have…
- Uploaded all of my assessment work for the Musical Language module.
- Suggested a topic for Kalie Shorr’s podcast, which she used, and then mentioned me and my music during it, which meant a lot to me.
- Followed the news about the riots at the Capitol building in Washington D.C.
- Started building my family tree on AncestryDNA and learning about who my relatives are, especially on my father’s side. This included messaging with distant relatives (cousins multiple times removed, for example), which was a pretty surreal experience.
- Listened to and fell in love with the bonus tracks from Taylor Swift’s evermore.
- Started a new (very beautiful) subscription of Vitamin D supplement.
- Had a socially distanced chat and exchange of Christmas presents with one of my best friends.
- Had a bit of a reset therapy session: we caught up and then set some goals to work on.
- Had multiple writing sessions with Richard.
- Wrote and posted a blog post about the third semester of my Masters.
- Tested out a new method of overcoming my Trichotillomania: using a strip of elastic to tie my hand to my portable desk, preventing my pulling hand from reaching my hair.
- Finished my ADHD assessment and was diagnosed with ADHD, although it’s a complicated one as there is much overlap between Autism and ADHD.
- Had a Netflix party with some friends where we watched How To Train Your Dragon.
- Started my new university module, The Writer’s Voice (online, of course).
- Binge-watched The Wilds.
- Had a productive meeting with one of the careers team at my university.
- Had multiple writing sessions with my friend and coursemate, Luce.
- Watched and critiqued the first draft of the acoustic session videos.
- Watched the film, How It Ends.
- Watched the film, Ava.
- Due to technical issues, my friend, Aislin, and I wrote a song using basically texts and a google doc; and not only that, it was a song we loved and felt really proud of, regardless of the circumstances.
- Watched Joe Biden’s inauguration; I found it very inspiring and emotional.
- Had a consultation with an Occupational Therapist (via phone) for the pain in my hands.
- Continued with my therapy sessions.
- Worked on a couple of songs with my friend and coursemate, Dan.
- Got my AncestryDNA results back, which was really interesting in some ways and frustrating in others.
- Had a long catch up call with one of my best friends.
- Had my first session for a new mentoring programme.
- Had a meltdown after an unexpected change with a university class and ended up missing the class entirely.
- Watched the series, Tiny Pretty Things.
- Had a COVID test.
- Had my COVID test come back negative.
- Had multiple sessions with my friend and coursemate, Anna.
- Watched one of my best friends, Luce, do her second online show.
- Finished the acoustic session videos.
- Began Occupational Therapy for the pain in my hands.
- Wrote a blog post about the first year without our dog, Lucky.
- Wrote multiple songs by myself.
- Started FAWM – February Album Writing Month, a challenge to write fourteen songs in twenty eight days.
- Had a phone call with the Chronic Fatigue Service that proved to be not only unhelpful, but deeply troubling: we discovered that I’d never received the results of blood-work from two years ago that showed multiple (potentially dangerous) abnormalities that should’ve been investigated and he told me my case was too complicated for them, that they didn’t feel they could help me.
- Ran into a friend that I haven’t seen for ages and we planned a call and (online) movie night.
- Had an ECG: hypermobility can result in heart problems (in a small percentage of people) so I’ll have to have regular heart check ups.
- Had a writing session with my friend and coursemate, Amy.
- Continued to spread awareness of how ableist, offensive, and dangerous Sia’s film, Music, is.
- Posted my blog post about the first year with our lovely dog, Lucky.
- Watched the film, Peppermint.
- Celebrated the beginning of Taylor Swift releasing her rerecorded albums, starting with ‘Love Story (Taylor’s Version).’
- Wrote with my friend and coursemate, Harrison.
- Watched the film, The Dig.
- Had a long overdue movie night (in the middle of the day) and catch up with two of my best friends.
- Posted two blog posts on the same day about Trichotillomania. (x) (x)
- My Mum had her first COVID vaccination.
- Had a difficult video call with one of my tutors about one of the Masters modules, in which I got very upset.
- Watched Series 1 and 2 of The Bay.
- My Mum trimmed my fringe for me.
- Received the about-face makeup (by Halsey) I’d bought and tested it out; I particularly liked the matte lip product.
- Rewatched Criminal Minds from start to finish.
- Had several writing sessions with my new friend and coursemate, Phill.
- Received the Chronic Fatigue Service’s post-session report before they sent it to my GP and corrected all of the errors in it (such as when I was diagnosed with ASD).
- Watched the film, Taking Lives.
- Rewatched all three seasons of Absentia.
- Had another mentoring session, which was really thought-provoking and productive.
- My university had a reading week so I didn’t have any classes.
- Had a planning session with Richard after one of our writing sessions.
- Found the new COVID-19 plan announced on the 22nd February thoroughly unclear and confusing.
- Watched New Amsterdam Season 1.
- Wrote several songs based on fictional stories and characters, which isn’t my writing comfort zone but was really fun.
- Started watching Unforgotten Series 4; I’m ecstatic to have Nicola Walker on my screen again, especially playing such a great character, but given the end of the last series, I can’t help but worry that this will be the last.
- Had multiple sessions with my friend and coursemate, Simon.
- Watched the film, Escape From Pretoria.
- Completed FAWM (February Album Writing Month), actually writing 14 songs in less than 28 days.
- Had a socially distanced catch up with one of my oldest and best friends.
- Had a second COVID test.
- Did several Autism research studies (from home, of course).
- Dyed my hair.
- Had a writing session with my friend and coursemate, Joy.
- One of my best friends, Richard Marc, released his debut single, ‘Put It In A Postcard,’ which I helped write.
- Had my COVID test come back negative.
- Learned that my ECG had come back clear.
- Had official confirmation that I’ve been diagnosed with Hypermobile Ehlers-Danlos Syndrome.
- Had a meeting with uni staff to discuss the options around the process of changing my antidepressants in order to take medication for my ADHD.
- Watched New Amsterdam Season 2.
- Met a potential DSA mentor (it didn’t work out).
- Was unexpectedly triggered during a seminar and got extremely upset, although I was somehow able to pull myself together enough to manage the class.
- Bought tickets for me and my family to see Tim Minchin when he (hopefully) tours the UK at the end of the year.
- Announced the Honest EP (Sunburst Sessions).
- Fell down the stairs but fortunately wasn’t too badly banged up.
- Sweep had to go to the vet because she seemed to be having trouble moving around comfortably but the vet wasn’t worried and thought she’d probably been knocked around in all the wind we’ve been having and has given her some painkillers. We also asked if she had any guesses as to what breed Sweep is since we have no idea and her guess is Long Haired Domestic Cat with potentially some Norwegian Forest Cat, so that’s what we’re going with unless we decide to do one of those pet DNA tests.
- Had a good catch up call with one of my oldest friends.
- Caught up with The Grammys, celebrated Taylor Swift’s folklore winning Album of the Year, and cried over all of the acceptance speeches.
- Watched The One (Season 1).
- Had a particularly good response in class to one of my songs, which is one of my favourite songs I’ve written recently.
- Had a really productive meeting with my course leader about my Masters final project.
- Had an upsetting and thoroughly unhelpful appointment with a specialist I’d been referred to.
- Had another set of blood tests – I’ve completely forgotten what they’re for or who requested them with so many people involved right now but they might give us more insight into my fatigue.
- Posted the first of the Honest EP acoustic sessions, ‘Bad Night (Sunburst Sessions)’.
- Learned about Travis Meadows’ surgery, donated to the gofundme, and shared the link.
- Watched one of my best friends, Luce, do an awesome online show.
- Posted my blog post about being diagnosed with ADHD.
- Watched Creating The Queen’s Gambit, which just made me want to watch the show again.
- Joined the judging panel for a songwriting competition.
- Screeched at the penultimate episode of Unforgotten Series 4.
- After a really fascinating seminar on Jungian archetypes, I spent hours reading more about them.
- Suddenly found out quite a lot about my Dad’s side of the family, which was amazing but pretty overwhelming.
- Had another meeting with one of the tutors to fine tune the approach to my Masters final project.
- Did an interview with an Autism publication.
- Attended Betsy Lane’s Zoom party to celebrate her (awesome) new single, ‘Plan For Paris.’
- Rewrote my professional bio, or attempted to at least.
- Had a long phone call with one of my best friends, which I think I really needed (plus she said something to me that may be the most special and important thing anyone has ever said to me).
- Worked on multiple blog posts for World Autism Awareness Week 2021.
- Had an excited little freak out about Lexie Grey (played by Chyler Leigh) appearing in Grey’s Anatomy again, even though I’m not watching the show at the moment (I just can’t manage living the pandemic and watching entertainment about it – but I loved Lexie so I look forward to watching it one day).
- Worked with Richard on my next release.
- I posted the second video in my acoustic session series, ‘Clarity (Sunburst Sessions).’
- Had a lovely, long call with one of my best friends.
- Received a late Christmas gift from one of my parents: a vinyl of the Honest EP!
- Got a very sweet comment from Natalie Hemby (one of my favourite songwriters) on Instagram.
- Wrote and submitted a research proposal for a conference.
- Got my first COVID vaccine!
- *SPOILER ALERT* Was deeply, deeply upset when Cassie died in the Unforgotten finale – I’m not sure I’ll ever feel the same way about the show and I don’t think I’ll be able to watch the next series.
- Wrote a song about grief called ‘Incomplete,’ inspired by Unforgotten but informed by my own experience.
- Had the initial meeting about the next and final module of the Masters, called The Major Repertoire Project.
- Worked on a really special song with my friend and coursemate, Anna.
- Went to a drop-in session (online) with my tutor to get some advice on my assessment work.
- Posted the third video in my acoustic session series, ‘Sounds Like Hope (Sunburst Sessions).’
- Had several video calls with my friend, Luce, where we worked on our songs for our assessment portfolios.
- My Mum cut my fringe again. It was alarmingly short this time.
- Put up a blog post for every day of Autism Awareness Week.
- Had my last workshop of the semester, which felt quite emotional.
- The research proposal that I submitted for the conference was accepted!
- Celebrated Taylor Swift re-releasing her album Fearless as Fearless (Taylor’s Version).
- Posted the fourth video in my acoustic session series, ‘Back To Life (Sunburst Sessions).’
- Rewatched The Wilds while I worked on various things.
- Started watching The Shires’ online concert but couldn’t finish it because of family commitments.
- Got some really exciting news about a creative project I’ve been involved with (I can’t talk about it yet since it isn’t my project to announce).
- Got a new fidget toy that also seems to be complimentary to my Occupational Therapy exercises.
- Finished my marking for the songwriting competition.
- Rewatched Dare Me while I was working on various tasks.
- Met and had my first discussion with my Major Repertoire Project (the final module and project of the Masters) supervisor.
- Posted the fifth and final video in my acoustic session series, ‘Honest (Sunburst Sessions).’
- Ended up spending the day in A&E after three days with a migraine had my doctor concerned that I might be experiencing side effects from my COVID vaccine.
- Dyed my hair again.
- Finished my coursework for The Writer’s Voice module.
- Worked on a song with my friend and coursemate, Alessandro, which incidentally meant that I’d written with every person in the group.
- Submitted my coursework for The Writer’s Voice module.
- Celebrated one of my parents’ birthdays.
- Attended several (online) networking meetings organised by my university.
- Rewatched Blood & Water (Series 1).
- Upped my Occupational Therapy regimen.
- Got a haircut for the first time in MONTHS.
- Had another migraine that lasted for several days.
- Released the Honest EP (The Sunburst Sessions).
- Had a very distressing and unhelpful follow up appointment (by phone) with a rheumatologist (different from the original one).
- Hit a stumbling block in getting treatment for my ADHD.
As I said in the last part of this list, hopefully there won’t be reason to continue this post; hopefully there won’t be any more lockdowns. But I guess only time will tell. I’ve found it strangely comforting to keep this list; it’s kind of like a time capsule for these strange periods of time, if that makes sense.
I hope you’re all keeping safe and well and I’ll see you in the next post.
Category: adhd, autism, covid-19 pandemic, death, diagnosis, heds, medication, meltdowns, mental health, music, tips, trichotillomania, university, video, writing Tagged: a&e, about-face, absentia, acoustic ep, acoustic sessions, adhd, adhd diagnosis, adhd medication, ancestry, ancestrydna, attention deficit hyperactivity disorder, ava, betsy lane, birthday, blood & water, cat family, christmas present, chronic fatigue service, chyler leigh, collaboration, coronavirus, covid test, covid vaccination, covid vaccine, covid-19, cowriter, cowriting, cowriting session, creating the queen's gambit, criminal minds, dare me, dbt, dialectical behaviour therapy, ecg, escape from pretoria, evermore, family history, fawm, fawm 2021, fearless (taylor's version), february album writing month, film, films, folklore, friends, grammys 2021, grey's anatomy, grief, grief anniversary, haircut, halsey, heds, honest ep, honest ep (sunburst sessions), hospital, how it ends, how to train your dragon, hypermobile ehlers danlos syndrome, hypermobility, inattentive type, interview, kalie shorr, lexie grey, lockdown, lockdown 2021, lockdown 3.0, luce, masters, masters degree, masters degree in songwriting, masters degree year two, masters part time, medical trauma, medication, meltdown, migraine, movies, my cat, my cats, my dog, natalie hemby, new amsterdam, new music, new music release, new music uk, new single, nicola walker, occupational therapy, online concert, part time masters student, peppermint, politics, put it in a postcard, remote writing session, research conference, rheumatologist, rheumatology follow up, richard marc, social distancing, songwriter, songwriting, songwriting competition, sunburst sessions, taking lives, taylor swift, the bay, the dig, the one, the one netflix, the queen's gambit, the shires, the wilds, therapy, tim minchin, tiny pretty things, travis meadows, trich, trichotillomania, triggered, tv show, unforgotten, university, us politics, world autism awareness week, world autism awareness week 2021

About Me
Hi! I’m Lauren Alex Hooper. Welcome to my little blog! I write about living with Autism Spectrum Disorder (ASD), ADHD (Inattentive Type), and Hypermobile Ehlers-Danlos Syndrome (hEDS), as well as several mental health issues.
I’m a singer-songwriter (it’s my biggest special interest and I have both a BA and MA in songwriting) so I’ll probably write a bit about that too.
My first single, ‘Invisible,’ is on all platforms, with all proceeds going to Young Minds.
My debut EP, Honest, is available on all platforms, with a limited physical run at Resident Music in Brighton.
I’m currently working on an album about my experiences as an autistic woman.
Links
Categories
Recent Posts
Archives
- January 2026 (1)
- December 2025 (1)
- August 2025 (1)
- July 2025 (1)
- June 2025 (4)
- May 2025 (3)
- April 2025 (2)
- March 2025 (1)
- February 2025 (1)
- January 2025 (1)
- December 2024 (2)
- November 2024 (1)
- October 2024 (1)
- July 2024 (1)
- May 2024 (1)
- April 2024 (3)
- March 2024 (1)
- January 2024 (1)
- December 2023 (4)
- November 2023 (6)
- October 2023 (5)
- September 2023 (6)
- August 2023 (4)
- July 2023 (5)
- June 2023 (5)
- May 2023 (7)
- April 2023 (4)
- December 2022 (4)
- November 2022 (1)
- October 2022 (1)
- September 2022 (1)
- August 2022 (3)
- June 2022 (2)
- May 2022 (6)
- April 2022 (10)
- March 2022 (9)
- February 2022 (3)
- January 2022 (1)
- December 2021 (7)
- November 2021 (5)
- October 2021 (7)
- September 2021 (4)
- August 2021 (1)
- July 2021 (2)
- June 2021 (4)
- May 2021 (10)
- April 2021 (11)
- March 2021 (14)
- February 2021 (6)
- January 2021 (6)
- December 2020 (8)
- November 2020 (9)
- October 2020 (8)
- September 2020 (10)
- August 2020 (8)
- July 2020 (4)
- June 2020 (6)
- May 2020 (8)
- April 2020 (7)
- March 2020 (9)
- February 2020 (5)
- January 2020 (7)
- December 2019 (7)
- November 2019 (1)
- October 2019 (1)
- August 2019 (1)
- July 2019 (2)
- June 2019 (3)
- May 2019 (5)
- April 2019 (5)
- March 2019 (5)
- February 2019 (6)
- January 2019 (5)
- December 2018 (7)
- November 2018 (3)
- October 2018 (5)
- September 2018 (5)
- August 2018 (5)
- July 2018 (9)
- June 2018 (7)
- May 2018 (7)
- April 2018 (6)
- March 2018 (11)
- February 2018 (5)
- January 2018 (6)
- December 2017 (7)
- November 2017 (7)
- October 2017 (7)
- September 2017 (6)
- August 2017 (5)
About Me
Hi! I’m Lauren Alex Hooper. Welcome to my little blog! I write about living with Autism Spectrum Disorder (ASD), ADHD (Inattentive Type), and Hypermobile Ehlers-Danlos Syndrome (hEDS), as well as several mental health issues.
I’m a singer-songwriter (it’s my biggest special interest and I have both a BA and MA in songwriting) so I’ll probably write a bit about that too.
My first single, ‘Invisible,’ is on all platforms, with all proceeds going to Young Minds.
My debut EP, Honest, is available on all platforms, with a limited physical run at Resident Music in Brighton.
I’m currently working on an album about my experiences as an autistic woman.
 Finding Hope
Finding Hope