It’s A New Dawn, It’s A New Day, It’s A New… Medication
Posted on March 12, 2022
TW: Mentions of self harm and suicidal thoughts.
In the last week of January, my psychiatrist told me to stop taking the Bupropion since it was so obviously having such a detrimental effect. In theory, after the wash out period was complete, I’d start taking a new antidepressant, Moclobemide. It’s an MAOI, like Phenelzine (the antidepressant that I’ve ever had the best response to – the only one I’ve had a halfway decent response to), so my psychiatrist thought it was the best option. But I was so depressed that I just couldn’t take it: knowing how these medications affect me, I just didn’t feel emotionally capable to handle the change.
But then, after a hellish few days and some kind of breakdown, I started taking Moclobemide. At that point, it was self preservation: I didn’t want to but I knew that I couldn’t keep feeling that awful – or worse – because something terrible was going to happen if something didn’t change.
This change was somewhat complicated by the fact that I was taking other medications at the same time. I was taking a lot of Diazepam with my anxiety so bad and I was also taking 20mg of Propranolol (recommended for anxiety and POTS – which was diagnosed by a cardiologist after a first round of tests – although I’m not sure it’s doing anything for either).
As is always the case with posts about medication, this is just my experience. Please don’t start, change, or stop taking any medications without the advice and support of a medical professional.
WEEK 1 (150mg twice daily)
The first week was bad. I was completely overwhelmed by my anxiety and needed constant Diazepam to be even vaguely functional, just to get out of bed. I was very depressed, feeling exhausted and hopeless and worn down. I was still having thoughts about self harm and suicide although not as much as I had been but I just felt utterly overwhelmed, by everything the world wants from me. Life just felt like too much.
I was still struggling to fall asleep (there was one night when I was still awake at seven thirty am). My sleep schedule was completely fucked up; I was almost nocturnal. And even then, I was falling asleep in the day, regardless of how hard I tried not to. As I said, it was a whole mess. I was exhausted all of the time.
My struggles with food continued too. I could barely eat and on the rare occasion where I did feel able to eat, nothing appealed – at all – or satisfied the feeling. But between my mental health and my sleep issues, food felt like the least of my problems.
I also spent more than half the week with at least a low level migraine, which wasn’t exactly pleasant.

WEEK 2
The second week was also pretty tough, although in a few different ways.
I was still feeling very anxious – the Diazepam was only doing so much – and my depression was still very present. I just couldn’t engage. I was miserable. I felt very overwhelmed; life just felt like it was too much.
At the beginning of the second week, I started taking Temazepam – prescribed by my GP – to help with my sleep. It gave me a couple of good nights but after that it didn’t seem to do much. Most nights, I was still awake for hours and struggling up in the afternoons; waking up was miserable. I was exhausted and sleepy and kept falling asleep in the day, despite drinking Red Bull, something I haven’t felt I needed in ages.
I did have one pretty intense day: despite only getting about three hours sleep, I was up early and writing a song from start to finish – something I haven’t been able to do in months. It’s usually a sign of how good or bad my mental health is: things are getting bad if I can’t write. I’m not jumping for joy just yet but I am cautiously optimistic that if this is possible, things are improving. I felt really good for a couple of hours but then all of the bad stuff crept in again: I went to bed feeling exhausted and overwhelmed by my anxiety and depression.
At the end of the week, I spent two days in and out of a hospital in London, having tests done (I wasn’t taking the Propranolol for a few days as advised so that it wouldn’t affect the results). Just being in the hospital and the staff’s general lack of understanding around Autism was stressful and frustrating and exhausting. The first day was quiet but it was hard to relax with the blood pressure monitor going off every twenty minutes. The second day was more involved with more than three hours of tests. It was exhausting – I could barely stay awake for the rest of the day – and my whole body hurt afterwards, so badly that even getting upstairs when we got home was a struggle. I don’t have a whole lot of faith that these tests will show anything different than the first round (which resulted in the POTS diagnosis) or in medical tests in general anymore but I guess we’ll find out what they say in a few weeks.

WEEK 3
At the beginning of the week, I officially gave up on Temazepam since it didn’t really seem to be doing anything. My GP had prescribed melatonin for when the Temazepam ran out so, with her blessing, I started taking that instead. It definitely improved my ability to sleep: after months of being awake for hours on end, I was falling asleep within half an hour every night. But I was still sleeping late – into the afternoon – and feeling sleepy in the day. I had several RedBulls in a week for the first time in months, which is a step backwards that I’m not happy about. I don’t know whether it was the melatonin or a side effect of the Moclobemide (not unlikely since I had the same side effect with Phenelzine) but, regardless, I hate it. This was one of the reasons I was so excited to try the ADHD meds; I thought I might finally feel something other than exhausted or sleepy or tired.
My chronic pain kicked up again, which was deeply unpleasant. My whole body hurt all week: every joint felt ache-y and crunchy and grind-y. I took painkillers throughout the day but the pain woke me up at night almost every night. But the only painkillers that help are ones that I can only take for a few days at a time and when those three days ran out, I was back to Ibuprofen and Paracetamol – neither of them do much – which was miserable and so frustrating: this has been going on – on and off – for almost two years and all I have are sporadic three day periods where I’m somewhat pain-free. The lack of progress is enough to reduce me to tears.
Mental health wise, things were up and down. Some days were okay and I actually got things done for the first time in ages, but some days were really hard. My anxiety was still bad and I was restless and uneasy; I didn’t know what to do with myself. I just felt like I was making everything I worked on worse. I was depressed, feeling overwhelmed and hopeless.

WEEK 4 (450mg daily)
I was sleeping but sleeping restlessly and waking up a lot. And come morning, it was such a struggle to wake up. I would fall asleep again and again; staying awake felt impossible. I don’t know if that’s the melatonin or something else but it’s pretty miserable. I feel like I cannot open my eyes, cannot make my hands work. It’s not fun. At the other end of the day, things are generally better. It can take a while to get to sleep but it’s nothing like it used to be. It can take a while to get comfortable, wind down, relax but I’m still getting to sleep easier than I was without the melatonin.
In the daytime, I was getting sleepy within an hour of getting up and drinking Red Bull almost daily again. It’s not something I want to make a habit of but I was just too tired to figure out what the right thing to do was so I just focussed on getting through the day. But even with the Red Bull, I was tired and sleepy and all I wanted to do was close my eyes. Again, I don’t know if this is the melatonin or the Moclobemide but either way, I don’t know what to do. If it’s the melatonin, I can stop taking that and hope my sleep stays okay but if it’s the Moclobemide, then I’m pretty stuck. I really don’t want to spend my whole life feeling tired and sleepy because this is the only medication that works.
I’ve started working again – a bit, given how unpredictable everything’s been recently – after being completely unable to since the end of last year. That’s been good and hard (and completely exhausting) in equal measure, socialising too. It’s nice to be in contact with people again but so often, at the moment at least, it also makes me feel defective and broken. My friends are telling me about their jobs and their relationships and so on and all I have to talk about are the new meds I’m trying and the new therapy I’ve been thinking of trying. When you’ve been depressed and suicidal for the past four months, there aren’t a lot of light and fun conversation topics to reach for. So I just felt very lonely. I’m not putting that on my friends – I want to hear about their lives – but the disconnect is hard.
My chronic pain was bad too. My whole body was hurting, my joints aching, even my fingers. I still haven’t heard anything from the Pain Clinic so all I’ve got are over the counter painkillers that I can only take for a few days at a time. What I’m supposed to do on the other days, I don’t know; nothing else helps at all.
I’ve realised that I’ve been feeling cold a lot, pretty much all of the time. I’m not sure when it started but it’s been going on for a while. Even with a thick jumper, a scarf, wooly socks, and a blanket, I’m freezing.
Mentally, it was a tough week. I felt very anxious and overwhelmed. My depression was pretty bad too, although not as crippling as it has been, and I was just miserable really. I cried a lot. So, yeah, a tough week.
WEEK 5 (600mg)
My energy and sleep continues to be troublesome. It’s so hard to wake up in the morning: I keep going back to sleep, I can’t keep my eyes open, and my hands won’t work. I’ve found that eating right away helps but I hate it as a strategy; food is the last thing I want right after I wake up. Despite the difficulty, I have been managing to wake up earlier than I have been over the last few months and getting to sleep has been a bit easier (with the help of the melatonin – although it does sometimes feel like I have to focus really hard on falling asleep sleep, which seems to be somewhat counterproductive). But I was still very sleepy during the day, falling asleep accidentally a couple of times, and so tired, although it was a busier week. I was doing more, socialising more, and feeling everything more intensely. There were some really good moments but it was hard too.
And, of course, more activity has resulted in more pain. I’ve been in pain constantly but it’s gotten worse. Multiple long car journeys and more time on my feet has caused problems with my back; I’m sure that with time, sensible exercise, and slowly building up my stamina, things will get better but it’s really hard to be patient. The pain has also been really bad in my hands (from my elbows down to my finger joints), which instantly instills a cabin fever-like feeling inside my own skin. I’m still waiting to hear from the Pain Clinic but experience doesn’t exactly encourage high hopes for what they’ll come back with, if they ever do.
My mental health has been all over the place. Five weeks of this medication and I still don’t feel like I’ve got my head on straight. As I said, I’ve had some good moments this week but I’m still struggling, more than I feel like I should at five weeks of a medication. I’ve had a lot of anxiety and my depression is still very present. My suicidal thoughts aren’t as constant as they were but they are still there. I guess, I just would’ve hoped that, at this point, I’d be feeling better mentally. It’s hard to not lose hope.
So, I’ve been taking Moclobemide for five weeks and while things are very different from day one, I’m still not feeling great. My depression is still a constant, day-to-day battle, which is one thing if I’m waiting for medication to kick in and for it to get better but if this is it, it’s not enough. I’m grateful that things are better – that I can write songs again – but living like this is really, really hard. I just want to feel better. I don’t want every day to feel like a mountain that I have to climb. I guess, I just want to feel normal. Although, having said that, I don’t know if I even know what normal feels like.
Category: adhd, anxiety, autism, chronic fatigue, depression, emotions, food, heds, medication, mental health, music, self harm, sleep, suicide, treatment Tagged: adhd medication, antidepressants, anxiety, bupropion, caffeine, chronic fatigue, chronic pain, creative block, depression, diazepam, drowsiness, eds, heds, hypermobile ehlers danlos syndrome, hypermobility, insomnia, loss of appetite, maoi, maois, medication, mental health, mental illness, migraine, migraines, moclobemide, pain, pain clinic, pain management, pain medication, phenelzine, pots, propranolol, red bull, self harm, self injury, sleep, sleep schedule, sleep wake cycle, sleepiness, songwriting, suicidal, suicidal ideation, suicidal thoughts, suicide, temazepam, trigger, trigger warning, tw, writers block, writing
Vitamin D Deficiency
Posted on January 23, 2021
Back in October 2020, I had a long overdue blood test. I think it was actually supposed to be the test that told us whether I’d absorbed and responded properly to the iron infusion I’d had in June 2019 but with starting the Masters and then the pandemic, it had only just become possible.
Going out and going to the Doctors’ Surgery did cause me a lot of anxiety – I’m still struggling with going out and with feeling very vulnerable when I’m out – but the appointment felt very safe and very efficient. I was probably in and out in less than ten minutes. About a week later, we got the results back and my iron was within the normal range. So all good there. However, my Vitamin D levels were seriously low, so low that they wanted to take immediate action. I was prescribed Colecalciferol, a prescription Vitamin D supplement, and instructed to take one a day for ten weeks.
It wasn’t surprising to hear that my vitamin D was low. It’s not uncommon for autistic individuals to have low vitamin D levels and with the pandemic and lockdown, I was staying inside a lot more and therefore not getting as much sunlight as usual, let alone the sunlight I needed. So I wasn’t shocked. I was pretty wary about taking supplements though: my last attempt with supplements had rendered the anti-depressants I was taking at the time completely ineffective, leaving me in a deep, dark hole of depression. Even though I stopped taking the supplements immediately, the anti-depressants never worked again. So I was concerned that something similar might happen again and I’d lose the only consistent (and I use that word loosely) anti-depressant I had in my toolbox. But my doctor explained just how important it was to get my vitamin D up and despite my anxiety, I committed to taking them.
For the first three weeks, I didn’t feel any different. My sleep was as sporadic as ever and I was constantly tired, something that is very much linked with my anti-depressant medication but is also a symptom of a vitamin D deficiency. Week four passed and I still didn’t feel any change but my Mum felt that there had been a slight shift, in my day to day behaviour and my engagement in whatever I was doing. She couldn’t quantify or qualify it any more than that but she did have a feeling that something was slightly different. I was reluctant to believe her, not feeling it myself.
Weeks five and six were tough: I was constantly exhausted and incredibly depressed, although it wasn’t always noticeable, covered up by anxiety-induced busyness. I was sleeping a lot but I was still tired but by the end of that sixth week, I was starting to wonder if I felt different. It’s just so freaking difficult to tell when the change you’re watching out for is so gradual. I wasn’t sure, just cautiously optimistic.
I’d been instructed to go back to the doctors’ surgery for another blood test between four and six weeks to see how I was responding to the supplement. It was closer to six weeks given some difficulty getting an appointment but when it finally happened, it was quick and efficient, just like the first appointment.
During what was the seventh week of this period, I was still tired and sleepy but again, I was starting to think that it wasn’t quite as bad as it had been. It wasn’t drastically better but I did feel a slight – intangible, I guess – difference. But week eight gave me a real sign that things were changing. I was still fatigued easily, still had days where I was really sleepy but I suddenly noticed that I wasn’t needing to drink as much Red Bull as I had been. Ever since I started this round of anti-depressants, I’ve been relying on Red Bull to keep me awake during the day and when the vitamin D first showed up as problem, I was probably drinking three a day – more when I was commuting to university (and yes, I’m aware that this isn’t healthy and have a plan with my psychiatrist to address it, although that has been derailed somewhat by the pandemic). But during week eight, I realised that I was getting through the day on one, sometimes less. Still not super healthy, yes, but a really good step in the right direction. And if I wasn’t feeling like I needed them as much to stay awake, then I had to assume that my energy levels were improving, to some degree at least.
When the blood test results came back, they showed that my vitamin D levels were back within the normal range but still pretty low so my doctor wrote me a new prescription for the rest of the winter with potential for extending it throughout the duration of the pandemic. I’m grateful for that; it’s one worry off my mind at least.
My energy levels still aren’t great. But getting my vitamin D levels under control was never going to be ‘the fix.’ Fatigue is a constant in my life, between my anti-depressants, Chronic Fatigue Syndrome, and other health (physical and mental) problems. But that doesn’t mean I can’t improve my situation. Getting my vitamin D levels back up has helped, hopefully hydrotherapy will help, perhaps the next anti-depressant won’t have such bad side effects (whenever I have time to try a new one – mid-Masters isn’t exactly the perfect time, especially having just reached the modules I’ve been most excited for). Sometimes I need to rage and cry about the pretty constant tiredness, but most of the time I can look forward and focus on the next thing that could help.
Category: anxiety, chronic fatigue, covid-19 pandemic, medication, mental health, sleep Tagged: anti depressants, antidepressants, anxiety, asd, autism, autism spectrum disorder, autistic, autistic adult, autistic student, blood test, caffeine, cfs, chronic fatigue, chronic fatigue, colecalciferol, coronavirus, covid-19, depression, disturbed sleep, fatigue, hydrotherapy referral, insomnia, low vitamin d, mental health, pandemic, pandemic 2020, pandemic anxiety, physical health, red bull, redbull, sleep, sleep schedule, sleepiness, supplement, supplements, tired, vitamin d, vitamin d deficiency, vitamin deficiency
ME/CFS Research: Photo Diary (Pre Lockdown and During Lockdown)
Posted on September 26, 2020
Not long ago, I volunteered for a research study into ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome) and part of it involved keeping a photo diary as a visual representation for how my life is affected by my CFS. Obviously my life before the pandemic and my life now are quite different and so the researcher asked me to include pre-pandemic photos as well, to ensure that both experiences were recorded for the study. The collection of photos (and descriptions) I sent her was very long but I thought I’d do an abridged version to post here because it was a really interesting exercise.
(It’s worth noting that this was put together before I started back at university, hence why there aren’t any current references to classes or assignments.)
PRE-LOCKDOWN

1. During my BA, I frequently took naps in quiet corners of my university between classes and then at my best friend’s flat when he moved onto the same street as the university. I found the commuting exhausting and the classes were long (some of them three hours) and took a lot of concentration. By the end of the semester, I was often really struggling to wake up to go back for the next class. A few times, I slept straight through both my alarm and my class. Fortunately that only happened a couple of times!

2. I’m currently doing a Masters Degree in songwriting part time and pre-lockdown, I’d go up to London usually once or twice a week for lectures, workshops, and cowriting sessions. This is an example of one of the assignments we had during the first module, which was called Creative Process.

3. Because living alone would be too much for me – I wouldn’t have the energy to look after myself, let alone do anything more – I commute to university (pre-pandemic anyway), involving lots of underground travel and multiple train journeys a week, something that I find exhausting. This is one of the reasons I chose to do my Masters part time because it reduced the amount of travelling and therefore allowed me to spend more energy on the course/work rather than on travelling.
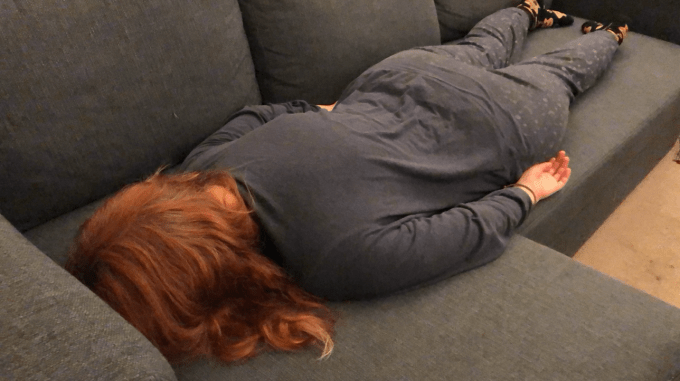
4. At the end of any day that involves hard work or anxiety, I’m utterly exhausted and usually end up horizontal on the sofa or going to bed as soon as I get home from wherever I am. In this instance, I’d just done the assessment presentation for the first module of my Masters – which I’d been incredibly anxious about – and was completely exhausted. Plus the day had involved practicing it in the morning as well as travelling to London and back. I was so tired that I could barely stay awake long enough to eat dinner before going to bed.

5. I spent most of my days out of uni on the sofa, working on music, my mental health blog, or catching up with my diary, a favourite movie or TV show on in the background because I work better with background noise. I’m usually joined by a cat or two.

6. As a singersongwriter, I try to perform as often as I can, both in terms of opportunity and having the energy (I once played three gigs in three days after which I could barely function for over a week because I’d just used up so much physical, mental, and emotional energy). That’s not a common problem – managing my energy around the amount of gigs – as there aren’t a huge number of opportunities with so many aspiring singers in the two cities I perform in, London and Brighton. I love performing. It’s the place I most feel myself, especially if I’m singing songs that I’ve written. I don’t feel any fatigue while I’m performing – I’m feeling so much joy that it’s like I’m flying – and I don’t feel any fatigue until the adrenaline wears off, anywhere between thirty minutes and several hours later.

7. Since getting an Autism Spectrum Disorder diagnosis, I’ve been able to get access to disabled seats at concerts, which does (in certain ways) improve my concert experience. It can be more stressful and it can make no difference at all but at the very least, it makes me feel better. I am in the disabled section and therefore no one can judge me or think that I don’t deserve to be at the show because I’m not dancing around, not ‘enjoying myself enough.’ That makes me feel more able to sit as I need to, which does make the concert experience easier on me and my body. Having said that, I’m not always so sensible out of sheer enthusiasm.

8. Before the pandemic, my best friend, Richard, and I had almost weekly writing and production sessions. My current EP was made almost entirely by the two of us in various rooms in the various places we’ve lived in over the last few years. These sessions are so fun and invigorating and even when it’s a struggle to find the right words or get the production to sound exactly how I want it to sound, it always feels right. I often feel very drained afterwards because it involves a lot of concentration and communication and we often work for four hours or more at a time. We have had sessions that last all day where I’m barely coherent by the end.
SINCE LOCKDOWN

1. We have five cats in the house and I’ve been spending a lot of time with them. They’ve always been really good for my anxiety – probably because they are so mindful and live so fully in the moment – but they’ve been an extra comfort during these stressful times. I always try to get a good cuddle in the evenings since I get particularly anxious before bed because I’ve been sleeping so badly and having lots of nightmares during lockdown.

2. I generally drink at least two Red Bulls a day to keep myself awake and somewhat alert, although I don’t think they work as well as they used to. I’m sleepy all the time, but whether that’s from the CFS or the side effects of my anti-depressants or both, I don’t know. I hate feeling like I need to drink it and I worry about the effects on my health but it’s currently the only way I can stay awake for at least most of the day. My Mum and I are investigating other options, or we were until the pandemic brought everything to halt. We haven’t given up though.

3. This is my usual day-to-day view at the moment. I have a desk designed for bed or sofa use so that I can work from the sofa, which is more comfortable for me than working at my desk since I’ve been have problems with pain during lockdown (I’ve been referred to various hospital departments but I’m still waiting for the appointments). I’m usually working on my laptop – on my mental health blog, on my diary, on music stuff, etc – and there’s usually a cat draped over me.

4. I usually have the TV on in the background because I seem to be more productive with familiar background noise, like a familiar TV show or movie. But I’ve also been watching new things during lockdown, both to escape from all of the stress around the pandemic but also as inspiration for my music as not much is happening in my personal life to draw from for songs. This is the very last episode of Agents of Shield, my favourite TV show and I was hugely sad to see it end although the ending was as perfect as the end of something you love can be.
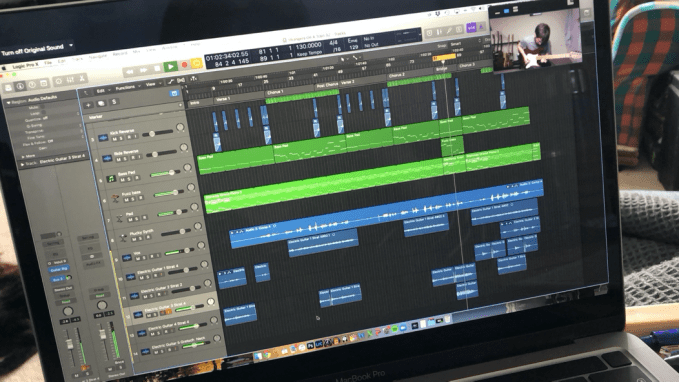
5. Since face-to-face writing sessions aren’t safe at this current time, I’ve been doing all of my writing sessions via Zoom. I’m currently doing about two a week, mostly with my writing partner, Richard. We alternate sessions: one on my songs and then one on his songs and so on. It’s harder work and not quite as fun or productive as a normal pre-pandemic session (who would’ve thought that not being able to point at something would trip up the creative process?) but it allows us to keep creating, which I’m grateful for. I’m always careful not to plan anything too difficult afterwards because these sessions are really draining and after about four hours, my ability to concentrate starts to fade.
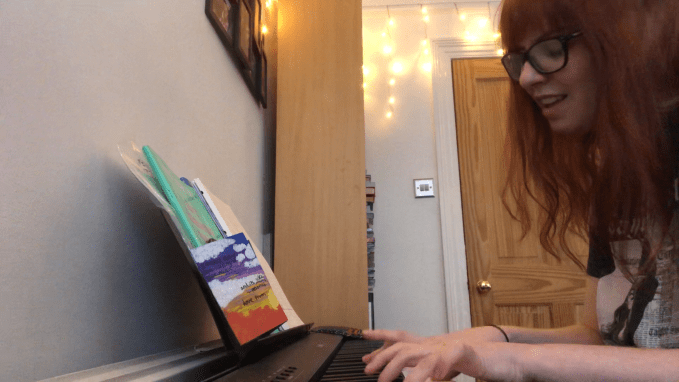
6. I’ve been playing a lot of piano during lockdown. It distracts me from all that’s going on, I want to improve my skills, and I just genuinely love playing, especially in the lower octaves. I find them very soothing. I can play for hours without noticing the passing time; it’s lovely. Playing and singing for hours is, of course, tiring but it’s worth it because I get so much enjoyment out of it.

7. Because of my fatigue, I spend a lot of time on the sofa, which can get boring and frustrating, but it’s not so bad when I have my Mum (she’s self-employed, primarily working from home – especially now) and the cats around.
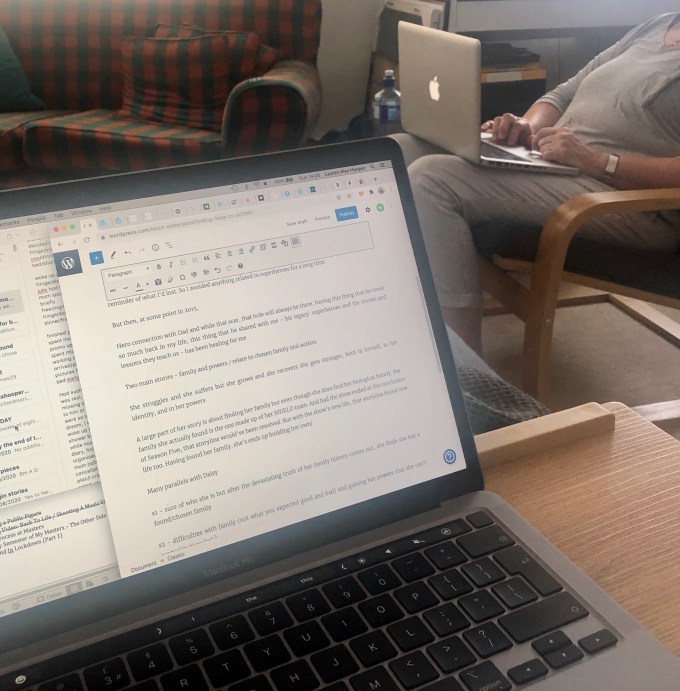
8. Most days consist of sitting on the sofa, working on my laptop. I’m writing a lot of posts for my mental health blog at the moment, preparing for when university starts again and I have less time to write. My Mum often does emails similarly, keeping me company even if we aren’t actively engaging with each other.
So that’s my condensed photo diary for the study. There are, of course, other areas of my life and other areas of my life that my CFS affects, like food and exercise but I don’t have any photos relating to those. For example, swimming is my main form of exercise but pre-pandemic I wouldn’t take my phone further than the locker room and since lockdown began, I’ve been struggling to find a way to swim that feels safe. I may have found one but I’m trying not to get too excited: I’ve missed it so much and I’m so desperate to get back to it, for my physical health, my mental health, and my relationship with my body. I was also reluctant to include other people; my exception was Richard because our work and social media presence are so intertwined. So there are obviously gaps but I tried my best to give an overview. Hopefully it will be a useful contribution to the research.
Category: about me, animals, anxiety, body image, chronic fatigue, covid-19 pandemic, depression, medication, mental health, music, research, sleep, university Tagged: agents of shield, asd, autism, autism spectrum disorder, autistic, blogging, caffeine, cat, cats, cfs, chloe bennet, chronic fatigue, chronic fatigue, commuting, concentration, concert, cowriting, daisy johnson, degree, desk, diary, diary writing, disability, disabled, energy, energy levels, exhaustion, family, fatigue, film, friends, inspiration, laptop, lockdown, lockdown 2020, logic pro x, masters degree, me/cfs, myalgic encephalomyelitis, pain, pandemic, pandemic 2020, pandemic anxiety, performing, photo diary, piano, production, recording, red bull, remote writing session, research, research study, research volunteer, richard marc, richard marc music, singer, singersongwriter, singersongwriter life, sleep, sleepiness, songwriter, songwriting, songwriting degree, songwriting session, student, tv show, university, work from home, writing session, zoom

About Me
Hi! I’m Lauren Alex Hooper. Welcome to my little blog! I write about living with Autism Spectrum Disorder (ASD), ADHD (Inattentive Type), and Hypermobile Ehlers-Danlos Syndrome (hEDS), as well as several mental health issues.
I’m a singer-songwriter (it’s my biggest special interest and I have both a BA and MA in songwriting) so I’ll probably write a bit about that too.
My first single, ‘Invisible,’ is on all platforms, with all proceeds going to Young Minds.
My debut EP, Honest, is available on all platforms, with a limited physical run at Resident Music in Brighton.
I’m currently working on an album about my experiences as an autistic woman.
Links
Categories
Recent Posts
Archives
- January 2026 (1)
- December 2025 (1)
- August 2025 (1)
- July 2025 (1)
- June 2025 (4)
- May 2025 (3)
- April 2025 (2)
- March 2025 (1)
- February 2025 (1)
- January 2025 (1)
- December 2024 (2)
- November 2024 (1)
- October 2024 (1)
- July 2024 (1)
- May 2024 (1)
- April 2024 (3)
- March 2024 (1)
- January 2024 (1)
- December 2023 (4)
- November 2023 (6)
- October 2023 (5)
- September 2023 (6)
- August 2023 (4)
- July 2023 (5)
- June 2023 (5)
- May 2023 (7)
- April 2023 (4)
- December 2022 (4)
- November 2022 (1)
- October 2022 (1)
- September 2022 (1)
- August 2022 (3)
- June 2022 (2)
- May 2022 (6)
- April 2022 (10)
- March 2022 (9)
- February 2022 (3)
- January 2022 (1)
- December 2021 (7)
- November 2021 (5)
- October 2021 (7)
- September 2021 (4)
- August 2021 (1)
- July 2021 (2)
- June 2021 (4)
- May 2021 (10)
- April 2021 (11)
- March 2021 (14)
- February 2021 (6)
- January 2021 (6)
- December 2020 (8)
- November 2020 (9)
- October 2020 (8)
- September 2020 (10)
- August 2020 (8)
- July 2020 (4)
- June 2020 (6)
- May 2020 (8)
- April 2020 (7)
- March 2020 (9)
- February 2020 (5)
- January 2020 (7)
- December 2019 (7)
- November 2019 (1)
- October 2019 (1)
- August 2019 (1)
- July 2019 (2)
- June 2019 (3)
- May 2019 (5)
- April 2019 (5)
- March 2019 (5)
- February 2019 (6)
- January 2019 (5)
- December 2018 (7)
- November 2018 (3)
- October 2018 (5)
- September 2018 (5)
- August 2018 (5)
- July 2018 (9)
- June 2018 (7)
- May 2018 (7)
- April 2018 (6)
- March 2018 (11)
- February 2018 (5)
- January 2018 (6)
- December 2017 (7)
- November 2017 (7)
- October 2017 (7)
- September 2017 (6)
- August 2017 (5)
About Me
Hi! I’m Lauren Alex Hooper. Welcome to my little blog! I write about living with Autism Spectrum Disorder (ASD), ADHD (Inattentive Type), and Hypermobile Ehlers-Danlos Syndrome (hEDS), as well as several mental health issues.
I’m a singer-songwriter (it’s my biggest special interest and I have both a BA and MA in songwriting) so I’ll probably write a bit about that too.
My first single, ‘Invisible,’ is on all platforms, with all proceeds going to Young Minds.
My debut EP, Honest, is available on all platforms, with a limited physical run at Resident Music in Brighton.
I’m currently working on an album about my experiences as an autistic woman.
 Finding Hope
Finding Hope
