2023 in Review
Posted on January 1, 2024
TW: Discussion of depression, self harm, and suicidal thoughts and ideation.
Much like last year, I have no idea how to sum up this year. I don’t think I have it in me to write a long post that involves such intense emotions and I think that, if I wait until I do, we might all be waiting a very long time so I’m just going to write until I can’t anymore and that’ll be that. It’s just too hard.
While there have been good moments (some of which can be seen in the collage below), it’s been a fucking painful year and it’s now the third New Year’s Eve that I’ve spent crippled by depression, suicidal thoughts, and overwhelming fear and dread around the future. I’m pretty sure I’m in full autistic burnout and I feel like I’m living in a fog. Last year, I think I described my depression as a drought but, this year, I think the better metaphor is drowning: I feel like I’m drowning in this depression and I have so little energy left that staying afloat is feeling more and more impossible. I’m so tired. I’m tired of trying so hard, of feeling like I’m not trying hard enough; I’m tired of feeling this way, of feeling like things will never get better, like there’s no point in even trying to feel better because there’s nothing worth feeling better for. It just feels like there’s so much bad in the world, so much agony, that it isn’t a world I want to live in. I feel broken; I feel like a prime example of a defective human being. There have been good things, like I said, but it seems like they can never just be good things: there’s always so much bad or hard twisted up in them that enjoying them isn’t as straightforward as it sounds. I miss feeling safe. I miss feeling safe to feel things.
A big, hard part of this year has been that I started taking Phenelzine again, for the third time. I didn’t want to and I felt coerced by the circumstances to take it. I was so angry about it all that I made potentially my most dramatic, self destructive move so far: I cut my face and then, when it got infected, I was so reluctant to treat it that I’ve ended up with a fairly visible scar. The most confusing part of it was that, even though I didn’t want anyone to bring it up, I was surprised that no one did; it seemed like the kind of thing that would trigger some alarm. Just as I imagined voicing consistent suicidal would but no one’s really commented on that either. It only makes the experience more isolating and lonely. But back to the Phenelzine: while it helped me get out of bed and go out now and then, it hasn’t had the same impact that it’s previously had on my mood, even on the higher dose. And that means that I’ve officially run out of medication options. I’ve been going to therapy consistently, for the most part, but I feel like it’s getting harder and harder; there have been sessions where I’ve left feeling traumatised. We’ll be trying something different in the new year but I’m struggling to feel hopeful, but that’s not specific to just therapy.
I look at the collage I made for this year and although I remember each of these moments, I feel disconnected from them; the emotions feel dulled. A lot has happened, somewhat to my surprise…
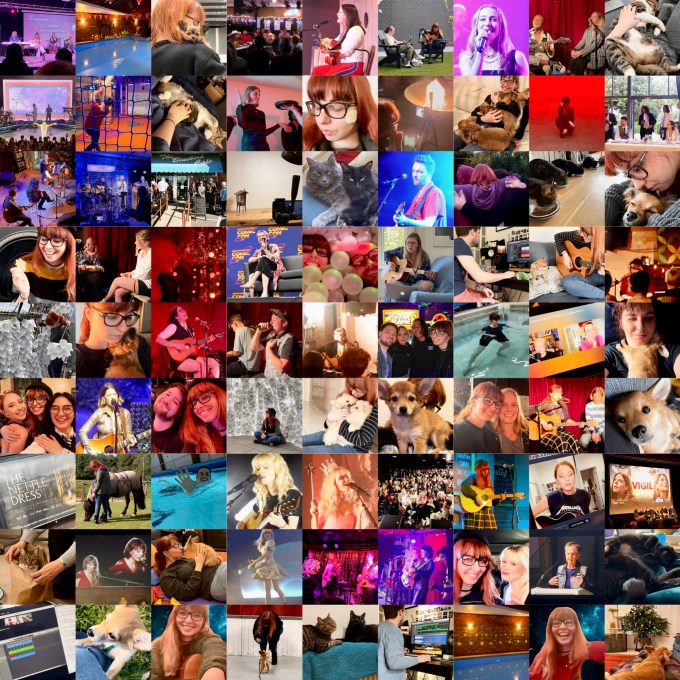
I went to multiple small shows; I went to hydrotherapy religiously and started physiotherapy; I got adopted by a puppy and then had my heart broken when she was taken away; I went to Nashville for Tin Pan South; my application for an Autism Service Dog was successful; I released my single, ‘House on Fire,’ as well as creating all of the visuals for it; I was diagnosed with Fibromyalgia; I went to art exhibitions (and even helped to build my favourite art piece, Breathing Room); I hung out with friends, online and in real life; I travelled to Germany for the wedding of one of my best friends and was reunited with multiple friends that I hadn’t seen in years; I got to hang out with some of my American friends when they performed here; I fought for Taylor Swift tickets; I had my heart broken again when the rescue puppy we applied for was homed with someone else; I went to some amazing concerts; I met Amanda Tapping again and she’s still one of the most wonderful people I’ve ever known; I started performing again; I read books and watched movies and TV shows that are now among my favourites; I adopted a puppy (which still doesn’t sound real to me); I swam 5km for Mind, raising over £600; I went to multiple Maisie Peters shows and got to meet her too; one of my cats got very sick and we had to nurse her back to health; my aunt died; I changed heart medications; and I worked on lots of different musical and academic work. I know all of these things happened; I remember them clearly but it’s like watching them play on a screen. I know these memories are mine but they don’t feel like mine. It’s weird and sad.
I’m so tired. I’m tired of masking but I don’t know how to stop. I feel broken – physically, mentally, and emotionally – but as hard as I try, it never feels like enough. Over ten years later, it should be getting better not worse, right?
I don’t know what else to say. Life feels increasingly scary, internally and externally, and I just feel too broken to manage. I don’t know how people walk around without all of the fear and grief and anxiety that I do, that I see as such an intrinsic part of being human. As I wrote last year, “I don’t know what tomorrow brings. I don’t know what I want it to. I didn’t want this year. I didn’t expect to still be here and I’m not happy or pleased or grateful for that. I feel pathetic and stupid and cowardly; I feel broken beyond repair. I feel frozen, overwhelmed by all of these big feelings. If feelings could kill you, I think these would have.“
Category: animals, anxiety, autism, chronic fatigue, chronic pain, death, depression, diagnosis, emotions, event, family, favourites, heds, hydrotherapy, medication, mental health, pots, self harm, suicide, therapy, treatment Tagged: 2023, actuallyautistic, amanda tapping, antidepressants, asd, autism, autism spectrum disorder, autistic, autistic burnout, autistic singersongwriter, charity, dbt, depression, dialectical behaviour therapy, ehlers danlos syndrome, family, fibromyalgia, heds, hydrotherapy, hypermobile ehlers danlos syndrome, maisie peters, maois, medication, mental health, mental illness, monoamine oxidase inhibitors, new year, new years eve, phenelzine, physiotherapy, radically open dialectical behaviour therapy, rodbt, self esteem, self harm, self injury, self loathing, singersongwriter, songwriter, suicidal ideation, suicidal thoughts, taylor swift, therapy, treatment resistant depression, trigger, trigger warning, year in review
2023 in Songs
Posted on December 28, 2023
TW: Mentions of depression, suicidal ideation, and unspecified trauma.
This year, with the help of Phenelzine, I fell in love with music again, which has brought me so much joy. It did, of course, also make it even harder than previous years to narrow down the songs for this list. In an earlier post, I wrote this: “It’s so easy for time to make things blurry and for songs to transcend time that I love being able to see exactly when songs impacted my life and what they meant to me. I kind of love the idea of looking back one day – sometime in the future – and knowing which exact songs I connected to, rather than just having a vague sense of which artists and albums I loved.” I still really relate to it and it felt appropriate after what feels like so much time lost in the haze of my depression over the last couple of years when I wasn’t really listening to music at all. But, as I said, things have been getting better and I’ve been able to connect with music again, to enjoy it; I’m not sure if I can express how grateful I am for that. I’ve missed it so much.
So, this is my playlist for 2023. I’ve made a corresponding playlist on Spotify so you can listen along if you’d like to – you can find it here.
1. She Used To Be Mine by Sara Bareilles
The new year began as the last one ended, with the feeling that I was suffocating under the weight of my depression. As last year’s post shows, I don’t really listen to music when I feel like this but Sara Bareilles is the one artist that can get through the fog; the one artist that I can listen to pain-free. ‘She Used To Be Mine’ came on (it’s a gorgeous song and Sara has the most incredible voice) and after this awful year (and change) I’ve had, the title lyric in particular – “she is gone but she used to be mine” – resonates so strongly. The person I was before all of this… I don’t feel like she’s mine anymore. I remember her but who I was then and who I am now are not the same people. Sometimes I think she might be gone.
Favourite Lyrics: “She’s imperfect but she tries / She is good but she lies / She is hard on herself / She is broken and won’t ask for help / She is messy but she’s kind / She is lonely most of the time / She is all of this mixed up / And baked in a beautiful pie / She is gone but she used to be mine” AND “It’s not what I asked for / Sometimes life just slips in through a back door / And carves out a person / And makes you believe it’s all true” AND “And you’re not what I asked for / If I’m honest I know I would give it all back / For a chance to start over / And rewrite an ending or two / For the girl that I knew” (but honestly the whole song is stunning).
2. Mountain With A View by Kelsea Ballerini
I love this whole EP so much that it was honestly really, really hard to choose just one song. ‘Blindsided’ and ‘Interlude’ rank very high up on my list but I think my absolute favourite has to be ‘Mountain With A View.’ I love the production – it creates such a gorgeous atmosphere, perfect for opening the project – and the soundscapes wrapped in it, the storm in the background giving it a heavy feeling but one that will eventually break and clear. Kelsea’s voice sounds incredible, gorgeous and warm and intimate, something that makes me feel like, as the listener, we are being let into her world and her heart in a way that we haven’t before. The melodies feel effortless, as if guided completely by the emotion, like a river moving through a landscape to the sea. The lyrics are delicate and vulnerable, with visceral (but beautiful) imagery and metaphors smoothly twisted together, like: “I’m wearin’ the ring still, but I think I’m lyin’ / Sometimes you forget yours, I think we’re done tryin'” and “I’ve shared all my secrets and I’ve paid for all my crimes / And our stars ain’t fallin’ back in line” and “I think that this is when I cut the ties / I think that this is when I set myself free / One day you’ll ask, ‘When was it over for you?’ // I’m takin’ the ring off, I’m finally cryin’ / Don’t try to find yours, no reason to fight it.” A heartbreaking detail is how she seems to become more and more certain of what she feels she has to do throughout the song, the lyrics shifting from “I should be missing you” and “I think we’re done trying” to “I can’t handle another year of you and I just bein’ fine” to “I’m taking the ring off, I’m finally crying” and “Don’t try to find yours, no reason to fight it.” That last chorus-bridge-chorus is just so heartbreaking as it all breaks down, as she accepts the end and the consequences of making that decision. My favourite lyric of the song, even if it makes my chest hurt (especially because of how Kelsea has talked about how painful her parents’ divorce was for her, how much it affected her), is “You’ll say I’m crazy for bein’ the one to leave / Scream, I’m just like my parents and givin’ up easy.” It’s so sad: if you love someone, it’s just so cruel to throw something like that in their face, something that you know will hurt so much. Including that in the song just feels so vulnerable and I’m touched by fact that she’s trusting us – her listeners – with something so personal and painful. I think it’s ultimately this openness and trust in her audience that makes this body of work so strong. Of all of her projects, this EP is easily my favourite so far and I doubt I’m alone in saying that it’s the best work she has produced to date.
(I also think it’s worth noting that the obvious title for this song, given the hook, is ‘Over For Me,’ which would’ve been a neat and petty match for Morgan Evans’ single, ‘Over For You.’ We know from interviews how angry that song made Kelsea, especially given that he released it before they were even officially divorced, so it would’ve been easy to be juvenile and use it to strike back at him but because she’s mature and sensitive and thoughtful about her art, she knew it was important for the art to stand on its own: to be about her experience and her feelings. It was always going to generate a certain level of gossip because they were a fairly public, celebrity couple but as far as I can tell she’s done a really good job of telling her story without feeding the gossip machine any more than absolutely necessary.)
Favourite Lyrics: “I’m wearin’ the ring still, but I think I’m lyin’ / Sometimes you forget yours, I think we’re done tryin’ / I realize you loved me much more at twenty-three / I think that this is when it’s over for me” AND “I’ve shared all my secrets and I’ve paid for all my crimes / And our stars ain’t fallin’ back in line” AND “I think that this is when I cut the tie loose / I think that this is when I set myself free / One day you’ll ask, ‘When was it over for you?’ // I’m takin’ the ring off, I’m finally cryin’ / Don’t try to find yours, no reason to fight it / You’ll say I’m crazy for bein’ the one to leave // Scream I’m just like my parents and givin’ up easy / But you never took that last flight to see me / Looks like our ending ain’t endin’ happily / I think that this is when it’s over for me”
3. SUBJECT TO CHANGE by Kelsea Ballerini // Let It Be Love by The Six One Five Collective
March was a month of really serious change so ‘SUBJECT TO CHANGE’ seemed like a very appropriate song to find myself obsessively listening to. After seeing Kelsea Ballerini live at the end of February, this song was just playing on a loop in my head; the song is just so fun and the melody is kind of intoxicating in how addictive it is. I can play it over and over for hours and be having just as good a time on the hundredth listen as I was on the first. From the lyrics to the melody to the production, it’s catchy and effervescent and uplifting, and I felt the joy trying to get in (even if I wasn’t ready for it yet).
My favourite part of the song is the second verse and pre-chorus. The verse feels so true to my life experience and it just resonates so deeply. As much as I love it though, the pre-chorus just gets me every time: “Thank God, I don’t know about tomorrow / Thank God, I take it day by day / Oh, I don’t think about the chapters / It’s all about turning the page.” It’s something that I really struggle with – trying to predict the future and act according to that imagined future – so those lyrics really speak to me and the way Kelsea sings them just warms my heart, like maybe I won’t always feel this way.
Favourite Lyrics: “If I’m honest / Growing up, it kind of hurts like hell / It’s chaotic, ironic / But it’s how I learn to find myself, yeah // Thank God, I don’t know about tomorrow / Thank God, I take it day by day / Oh, I don’t think about the chapters / It’s all about turning the page”
I heard Michael Logen play this brand new song at Tin Pan South in Nashville and I was in love with it by the end of the first chorus; it was so warm and hopeful and beautiful. The lyrics and melody were just gorgeous and the message of always, always coming back to love was so moving. And hearing the whole room sing the chorus – “Let it be love, love, love” – was an almost spiritual experience. I could’ve cried; it was such a beautiful, meaningful song. My depression still had its claws buried in me but I was starting to feel like connection might be possible again, that making music might be possible again. That’s what songs like this, what Nashville, gave me.
Favourite Lyrics: “If there’s only one thing that I’m known for / Just one legacy I leave behind / Just one word written over my hearthstone / Just one lesson I’ve learned in this life // Let it be love, love, love” AND “If it’s only one kingdom we’re building / Just one future we’re falling into / … // Let it be love, love, love” AND “Let it be love that holds us / Love that moulds us / Let it be love by which we are known / Let it be love that sees us / Love that frees us / Let it be love that leads us back home”
4. Too Much Of A Good Thing by Madeline Edwards // Lost The Breakup by Maisie Peters
I love Madeline Edwards’ album, Crashlanded, having being introduced to it and its stories when I heard her perform most of the songs at a round at Tin Pan South in Nashville. I loved it on the spot – the lyrics, the metaphors, the melodies, her voice, and then (later) the production – and I listened to it on repeat without a break for weeks. There are multiple songs that I absolutely adore – and could’ve happily chosen for this list – but it’s the last song, ‘Too Much Of A Good Thing,’ that speaks to me the most: it explores the idea that maybe good things can last, that they don’t have to run their course and come to an end as we’ve always been taught to expect (‘you can have too much of a good thing’ and ‘you can only have so much of a good thing’ and so on). She talked about how much that idea had impacted her life and how trying to have faith in the opposite, in the idea that good things can last, has helped her and enabled her to be present in the good when it’s happening. This is something that I really struggle with so this song really resonates with me and the more I listen to it, the more emotional it makes me. It’s simple and sweet, allowing you to focus on her voice, which is incredible, and the lyrics, which are poignant and uplifting.
Favourite Lyrics: “Well, life don’t always work like that / And hearts don’t have to break / And God don’t give to take it back / And dreams don’t have to fade / You can fly too close to the sun / And never melt your wings / And you can’t have too much of a good thing” AND “What if the love you want is the love you find?” AND “What if fear turns into scared of nothing? / You don’t have to let go of what you always wanted”
I think that the best pop songs are made up of catchy melodies, great lyrics that succinctly tell the story, and choruses that drive the point home. This song has all of those things and more. The verses give us the details of the story, of the break up; the prechoruses tee us up for the chorus while making her feelings for this guy scathingly clear; the choruses give us the biggest, most important pieces of the story without sacrificing the lyrical content or quality; and the bridge delivers a fun twist where, instead of winning the break up through revenge or spitefulness, she wins through getting over him and moving on with her life. I really love that narrative. I mean, I love a good revenge song but it’s really cool to have this different, more mature message, wrapped up in a fun pop song. The melodies are instant ear worms and the production pushes and pulls beautifully, the energy rising and falling in a way that carries you along effortlessly. It’s so much fun to sing along to and the hook – “oh, shit!” – is absolutely irresistible. It is quite possibly the most fun I’ve had listening to a song in a really long time. After struggling to feel joy for so long – to even remember what joy might feel like – it’s been beyond amazing to have so much fun listening to music again.
Favourite Lyrics: “I know I’m obsessed and / Right now, I might be a mess but / One day, you’re gonna wake up / And, oh shit, you lost the breakup / I’ll smile and you’ll have to face it / I’m the greatest love that you wasted / But, by then, I’ll be far away / And, oh shit, you lost the breakup” AND “But for now, I’m out in the dust / Falling apart / Oh, is she just like me? Yeah, I reckon / You got two types, Country and Western” AND “So, I’m feeling and I’m dealing with the heart you broke / While you do press-ups and repress us and take off her clothes / Here’s something if nothing else is still true / I’m the best thing that almost happened to you” AND “…and you’ll say / ‘Wow, hey, it’s been forever / Do you wanna get a drink, like together?’ / I say, ‘I’m kinda busy but, like, stay in touch?’ / I think, ‘oh shit, I won the breakup'”
5. Lie Better by Cassidy Daniels // Happy by Kesha
I fell in love with this song from the very first listen. Between the warm and emotive instrumentation, Cassidy’s gorgeous voice, and the lyrics – one heartbreaking punch in the gut after another – I was obsessed and listened to it on repeat, telling pretty much everyone I knew about this lyric or that one. The delicate acoustic guitar is absolutely perfect to represent that fragility of trying to hold yourself together after something has completely wrecked you and Cassidy has this beautiful, highly versatile voice, making her able to convey the heartbreak with such emotion. Hearing her like this was so moving to me because I’ve only really heard her sing really powerfully, an incredible belt that just filled the room, so it was really lovely to hear the other end of that spectrum, to hear her voice soft and vulnerable. The lyrics are – as usual – my favourite part and they are so fucking good. It’s really inspiring as a songwriter. The rhyming is so natural, especially in the bridge: “Wish you could lie better / Wishing that I never / Saw your true colours, wish you didn’t love her, wish you would’ve covered / Your lie better / Wish you could lie, lie better.” And the way she puts the universal experiences of those kinds of life changing moments – “I remember the day before the day I knew / When my forever was still forever with you,” for example – feels so organic but so deeply, painfully accurate. The whole song just sounds so real, like it just all spilled out in a moment of intense emotion.
Favourite Lyrics: “They say, ‘Ignorance is bliss’ / I guess it’s true, ’cause it’s gotta be better than this” AND “Wish you could lie better / Wishing that I never / Saw your true colours, wish you didn’t love her, wish you would’ve covered / Your lie better / Wish you could lie, lie better” AND “I remember the day before the day I knew / When my forever was still forever with you / I’d give anything to just go back / But a heart can’t forget when a heart attacks”
This song is so interesting to me, both following ‘Hate Me Harder’ and closing the album. And, of course, it’s gorgeous in its simplicity and vulnerability. The stripped back guitar really allows both Kesha’s voice and her lyrics to shine and they really do, closing out the album and this chapter of her life – this is the last album on her contract with her current label – on a very poignant note. I can understand why it’s (apparently) one of her favourites on the album. The song explores how her perspective has changed over time, how finding happiness has become her priority over everything else, a tough job for anyone but something that must feel like a particularly significant aspiration after everything she’s gone through in her life and career (most of which has been in the harsh light of the public eye): “If you asked me then where I wanted to be / It’d look something like this, living out my wildest of dreams / But life sometimes ain’t always what it seems / If you ask me now / All I’ve wanted to be / Is happy.” Having said that though, I found it very relatable…
- We’ve all been through tough stuff and given the traumatic experiences I’ve had and my struggles with mental illness and being neurodivergent, I can certainly relate to feeling like being happy could very well be an impossible goal.
- I love how the first verse – “What if none of this happened? / It’s nothing like I imagined it / What if I wasn’t this strong? / What if it all just went different?” – can be interpreted in different ways, particularly the line, “What if I wasn’t this strong?” The most obvious meaning is that, if she hadn’t been so strong, she wouldn’t have survived everything that’s happened to her. But an interpretation that I keep thinking about is how it almost sounds like it’s something she resents, like she couldn’t give up even if she wanted to, which is something I really, really relate to at the moment.
- The progression from “Time’s passing me by / Gotta just laugh so I don’t cry” to “Time’s passing me by / Gotta just laugh so I don’t die” is so heartbreaking.
- The lyric, “I remember when I was little / Before I knew that anyone could be evil / These egos, some people, playing with my innocence like at a casino,” has some of the most visceral imagery but it’s also so deeply relatable. I’m sure most of us – if not all of us – remember a moment when it became clear that the world was a lot crueler than we’d thought it was, when we were devastated by someone we trusted hurting us when we’d never imagined that they would.
The contrast between this song and ‘Hate Me Harder’ get me every single time. In ‘Hate Me Harder,’ she sings, “There’s nothing left that I haven’t heard / And I can take it, so make it hurt” and “Again and again and again and again, I’ll keep saying it over again / I’ve been there, I’ve done it, I’ve lived it, I’ve fucked it, I’d do it all over again / I’ll take it, I’ll take it, I’ll take it, I’ll take it, I already know that I can / Already know I can” but then, in ‘Happy,’ she sings, “What if none of this happened? / It’s nothing like I imagined it / […] / What if it all just went different?” and “There’s so many things I’d change but I can’t.” The two different points of view mirroring each other is just gut-wrenching, especially considering they are both delivered in such raw, vulnerable songs. When I listen to them, I think of ‘Hate Me Harder’ as the version of herself that she presents to the world, not a lie or a mask but just not her whole self, and then ‘Happy’ is the soft and vulnerable heart that she keeps protected from the world but chose to share with us on this track, on this album. Again, it’s not her whole self but it’s a really important part, especially when telling this chapter of her story. (It fascinates me how much we can learn about an artist from their albums – and discographies – which is why it makes me so angry and just heartbroken that the music industry is making it is so incredibly difficult for people to release them. Albums give you this beautiful chance to get to know an artist, to fall in love with them and become invested in them in a way that singles just can’t. Okay, tangent over. For now.) And that honesty and vulnerability, combined with the stripped down sound to let the lyrics take centre stage is why it is, in my opinion, the perfect closing track for the album and such a beautiful song.
Favourite Lyrics: “What if none of this happened? / It’s nothing like I imagined it / What if I wasn’t this strong? / What if it all just went different?” AND “Time’s passing me by / Gotta just laugh so I don’t cry” AND “I remember when I was little / Before I knew that anyone could be evil / These egos, some people, playing with my innocence like at a casino” AND “Time’s passing me by / Gotta just laugh so I don’t die”
Honourable mention to ‘Pathetic’ by Nick Wilson and both ‘We’re Not Friends’ and ‘Both’ by Ingrid Andress (I love her new album, Good Person, but these two songs have been really in my head because they’re just so good), both of whom I listened to a lot and saw live in May. They are amazing and the show was fantastic.
6. You’re Losing Me by Taylor Swift // Nervous System by Candi Carpenter
This song came out at the end of May and I’ve basically had it on repeat ever since even though it’s so gut-wrenchingly sad. At the time, we all thought it was a response to the breakup with Joe but clearly that relationship was much more complicated than we knew since Jack Antonoff revealed that it was written in December 2021. But anyway. The song is clearly about agonising over whether or not to end a relationship and the imagery she uses to depict that pain is beautiful, if deeply sad: “Remember lookin’ at this room, we loved it ’cause of the light / Now I just sit in the dark and wonder if it’s time,” “I sent you signals and bit my nails down to the quick / My face was gray, but you wouldn’t admit that we were sick,” “And the air is thick with loss and indecision / I know my pain is such an imposition,” etc. You can see those moments; it’s like you’re living them with her. You can feel her resignation, her exhaustion, the heaviness, the anger… She conveys the emotions so clearly, so smoothly; her writing skill is beyond incredible. The chorus is sparse and simple – “Stop, you’re losin’ me / Stop, you’re losin’ me / Stop, you’re losin’ me / I can’t find a pulse / My heart won’t start anymore / For you / ‘Cause you’re losin’ me” – but with the wordiness of the song, I think this only makes it more impactful, conveying the metaphor of the song more powerfully than a busier chorus would. The bridge is a stellar Swift-Antonoff classic that just keeps building and building until the emotion pours out like a waterfall. She questions how long they can go on in this unhappy state – “How long could we be a sad song / ‘Til we were too far gone to bring back to life? / I gave you all my best me’s, my endless empathy” – how she gave him everything, referencing military imagery, a heartbreaking throwback to ‘The Great War,’ a conflict that they managed to survive – “And all I did was bleed as I tried to be the bravest soldier / Fighting in only your army / Frontlines, don’t you ignore me.” She’s “the best thing at this party” but he still doesn’t seem to want her: “And I wouldn’t marry me either / A pathological people pleaser / Who only wanted you to see her.” Those lyrics always reminds me of ‘All Too Well (10 Minute Version) [From the Vault]’ and how she felt similarly unseen and misunderstood in that relationship: “The idea you had of me, who was she? / A never-needy, ever-lovely jewel whose shine reflects on you.” These specific phrases feel so personal, like someone knew exactly where to hit to make it hurt most; it’s heartbreaking. The final part of the bridge is so heart-wrenching, and all the more heart-wrenching for its simplicity: “And I’m fadin’, thinkin’ / Do something, babe, say something / Lose something, babe, risk something / Choose something, babe, I got nothing / To believe / Unless you’re choosin’ me / You’re losin’ me.” I swear it’s impossible not to scream along. The internal rhymes are so pleasing to the ear and I love the way the final “You’re losin’ me” fits into both the end of the bridge and the beginning of the final chorus. Production-wise, I love pretty much everything that Taylor and Jack do together but this isn’t one of my favourites; it’s poignant and atmospheric but, to my ears, it feels a little unfinished. I’d love to hear what it sounded like with production more in the vein of ‘The Great War’ or ‘Would’ve, Could’ve, Should’ve’ (although with a sparser arrangement).
Favourite Lyrics: “Remember looking at this room, we loved it ’cause of the light / Now I just sit in the dark and wonder if it’s time” AND “Stop, you’re losing me / I can’t find a pulse / My heart won’t start anymore / For you / ‘Cause you’re losing me” AND “I sent you signals and bit my nails down to the quick / My face was grey but you wouldn’t admit that we were sick // And the air is thick with loss and indecision / I know my pain is such an imposition” AND “And I wouldn’t marry me either / A pathological people-pleaser / Who only wanted you to see her” AND “Do something, babe, say something / Lose something, babe, risk something / Choose something, babe, I got nothing / To believe, unless you’re choosing me / You’re losing me”
I love Candi Carpenter and I could’ve chosen several from their EP for this slot; I relate so hard to multiple songs, in emotion if not always literally. But there’s something about ‘Nervous System’ – I think it’s because I just find it so relatable. I’m sorry but there is no lyric so relatable to me as the second verse of this song: “They say that life’s a party but I’ve always hated parties / I imagine a car wreck every time I touch my car keys / I don’t want to go anywhere / I’m a temperamental houseplant / Dehydrated, full of hatred / Cat hair on my sweatpants // When I check the CAPTCHA box that says I’m not a robot / I’m lying to myself and I’m lying to my laptop.” It’s just so hilariously me. And the choruses, both the original – “I have a nervous system / I’m nervous all time / I’m a lot like Hannibal, I’m just a cannibal / Eating myself alive / I have a nervous system” – and the extended final chorus – “These are fancy words // For my nervous system / I’m sorry it’s not more organised / It’s business as usual / I’m biting my cuticles / Literally eating myself alive / I have a nervous system / I’m nervous all time / I’m a lot like Hannibal, I’m just a cannibal / Eating myself alive / I have a nervous system” – are very me. The lyric-writing is so good, relatable and hilarious and whip-smart and the melody and rhyme-scheme make it such a satisfying song to listen to (and scream along to in the car). The production is so cool and so fun and Candi uses their voice with such skill: it’s so expressive and brings so much emotion… and just life to every track.
Favourite Lyrics: “I have a nervous system / I’m nervous all the time / I’m a lot like Hannibal / I’m just a cannibal / Eating myself alive / I have a nervous system” AND “I don’t want to go anywhere / I’m a temperamental houseplant / Dehydrated, full of hatred / Cat hair on my sweatpants” AND “When I check the CAPTCHA box that says I’m not a robot / I’m lying to myself and I’m lying to my laptop / I don’t wanna hand this down, I’m afraid to reproduce / I wonder if Sigmund Freud turned into his dad too” AND “These are fancy words // For my nervous system / I’m sorry it’s not more organised / It’s business as usual / I’m biting my cuticles / Literally eating myself alive / I have a nervous system”
7. History of Man by Maisie Peters // Castles Crumbling (Taylor’s Version) (From The Vault) by Taylor Swift
It’s safe to say that I’m obsessed with this album. It was so hard to choose just one to include here but the closer, ‘History of Man,’ is so powerful that I need to write about it. I love the muted production and the way it builds throughout the song but the lyrics are what really stand out (and I learned later that she wrote a lot of it just sitting at a piano, having decided not to write a song). There’s a lot in it but she seems to be telling the story of how, as hard as she tried, she couldn’t break the cycle of heartbreak that is as old as man itself; even pleading with the gods, that cycle can never be broken or rewritten. Before its release, she also described it like this: “This song is about so many things it’s hard to even distill into a tarot card paragraph. It’s about the power I feel as a songwriter, and the deep true magic I believe exists within love, even when that love has been lost. I wanted it to be the album closer because it encapsulates a lot of the themes I explore within [The Good Witch], but also because it sums up a large part of the feminine experience as I have felt it. This song feels deep and complex and important, like something bigger than me perhaps.” Throughout the song, she references history, mythology, bible stories, and symbolism to describe the break up of a relationship and the realisation that this story is so much older and bigger than she is, that hers is just the latest in an endless cycle. In the first verse, she establishes just how old love and heartbreak are and how, people have been falling in and out of love for as long as people have existed, through the biggest and smallest days in history: “Tale as old as honey / A moment everybody knows / Yeah, I’m sure there was heartbreak / Inside the walls of Jericho.” At the same time, she introduces her story, asking how her partner could just fall out of love with her, how he could hurt her so badly having loved her so much: “I couldn’t believe it / How you could just stop wanting me? / You burnt down Easter Island / As if it wasn’t sacred, as if it wasn’t sacred to me.” The imagery is beautiful and the references to all of these big, historic images give the song a powerful atmosphere and magnitude. In the chorus, she comes to the realisation that, no matter how hard she tries, this is something she can’t change: “I’ve seen it, in the poems and the sands / I’ve pleaded, with the powers and their plans / I tried to rewrite it but I can’t / It’s the history, the history of man.” This story of love and heartbreak has happened millions of times, a story that repeats over and over again: “She stays up, he’s sleeping like a lamb / She begs him, he says he doesn’t understand / She loves him, more than anyone ever has in the history, the history of man / It’s the history of man.” This is a burden shared by women, one that men just can’t understand, which makes the title – ‘History of Man’ – both ironic and heartbreaking. In the second verse, she seems to reference the story of Orpheus and Eurydice, where he must walk out of the Underworld without looking back in order to save her but he can’t resist looking and damns her to hell. The lyrics “You didn’t even falter / Didn’t look back once, did you?” seem to imply that he walked out easily, that he wasn’t even tempted to look back because he didn’t care, an idea she reinforces with the later lyric, “You walked out, oh / Without sweating.” She also references the story of Samson and Delilah – “So Samson blamed Delilah, but given half the chance I / I would have made him weaker too” – where Delilah betrayed Samson by cutting his hair and costing him his power. On Twitter, Maisie wrote that the lyrics referred to how she wished she could’ve made someone weaker so that they wouldn’t have left “as callously as they did.” She understands why Delilah acted as she did and would’ve done the same. It’s also interesting that Samson “blamed” Delilah when it was he who actually gave her the ability to hurt him, by sharing his secret, and could be interpreted to mean that this person had never shared enough of themself with Maisie to even let her hurt them. After another chorus, she digs even deeper into “the unending pain of the female experience” with the bridge: the first line, “He stole our youth and promised heaven,” refers to “older men taking advantage of younger women” and “the way we want to believe them, the way they know that and use it against us,” as Maisie explained on Twitter; “The men start wars yet Troy hates Helen” describes how, even though it was always the men that started wars, Helen was the one hated because she had power over men; “Women’s hearts are lethal weapons / Did you hold mine and feel threatened?” could easily refer to the way men are so quick to undermine women and to keep them down so that they will always be the ones holding the power, because a woman with power, something that Maisie is depicting here, is something they perceived as terrifying; the lyric, “Hear my lyrics, taste my venom,” sounds like Maisie’s own war cry, that people will hear what she has to say and recognise the power she holds (however the use of ‘venom’ could also be linked to the story of Eve being tempted by the snake and how, throughout history, women have been portrayed as liars and betrayers and villains); and the final lyric, “You are still my great obsession,” could imply that, despite the cruelty of men, women continue to obsess over the idea of falling in love, which can so often lead to pain and heartbreak. The final chorus begins as the previous ones do – “I’ve seen it, in the poems and the sands / I’ve pleaded, with the powers and their plans / I tried to rewrite it but I can’t / It’s the history, the history of man” – only to suddenly switch perspectives – “I stay up, you’re sleeping like a lamb / I beg you and you don’t understand” – implying that this time it’s her story that she’s telling, not a ubiquitous experience of women but her personal heartbreak, the latest in this long, long lineage. As she draws to the end of the song, she sings, “I hold on, I try to hold your hand / I save you a seat, and then you say you wanna stand,” which is a gut-wrenching image: she tried to hold onto the relationship and she did everything she could to save it, only to have it thrown back in her face, which brings them to the inevitable conclusion: “So you’ll lose me, the best you’ll ever have / It’s the history, the history of man.” If he treats her badly, she’ll walk away with a broken heart and he’ll be left alone, searching for someone ‘better’ and never realising that he had it but threw it away. And the story repeats. And repeats and repeats and repeats.
Favourite Lyrics: “Yeah, I’m sure there was heartbreak / Inside the walls of Jericho” AND “You burnt down Easter Island / As if it wasn’t sacred, as if it wasn’t sacred to me” AND “I’ve seen it, in the poems, in the sands / I’ve pleaded, with the powers and their plans / I tried to rewrite it but I can’t / It’s the history, the history of man” AND “He stole our youth and promised heaven / The men start wars yet Troy hates Helen / Women’s hearts are lethal weapons / Did you hold mine and feel threatened? / Hear my lyrics, taste my venom / You are still my great obsession” AND “I hold on, I try to hold your hand / I save you a seat, and then you say you wanna stand / So you’ll lose me, the best you’ll ever have / It’s the history, the history of man”
I love multiple vault tracks on this rerecording but I’m pretty sure ‘Castles Crumbling (Taylor’s Version) (From The Vault)’ is my favourite. It’s a beautifully written song with a really strong, powerful metaphor, one that is heartbreakingly similar to the one that Taylor uses in ‘Long Live.’ But rather than triumphant and euphoric, the imagery is haunting and atmospheric, with lyrics like: “Once, I had an empire in a golden age” and “And I feel like my castle’s crumbling down / And I watch all my bridges burn to the ground” and “Once, I was the great hope for a dynasty” and “Now they’re screaming at the palace front gates, used to chant my name.” It’s beautiful, in a desolate kind of way. The emotion, the self loathing, is so heartbreaking – “I will just let you down / You don’t wanna know me now” and “Crowds would hang on my words, and they trusted me / Their faith was strong, but I pushed it too far / I held that grudge ’til it tore me apart” and “And here I sit alone, behind walls of regret / Falling down like promises that I never kept” and “People look at me like I’m a monster / Now they’re screaming at the palace front gates, used to chant my name / Now they’re screaming that they hate me / Never wanted you to hate me” – and I find it so distressing to think about the fact that, even then – so relatively early in her career – Taylor had so much anxiety over her future; she was so young and so scared and it just makes me wish I could go back in time and hug her. By the time she calls herself a ‘monster’ in ‘Anti-Hero,’ she’s strong enough and she’s shared enough that we understand where she’s coming from, that it’s an insecurity rather than a belief, but that’s not necessarily clear here, coming from a not even twenty-one year old Taylor. The whole thing makes me emotional enough to cry. Her vocals are stunning, conveying such emotion and fragility, and Hayley Williams’ compliments her beautifully; the production is gorgeous too’ somehow both sparse and anthemic.
Favourite Lyrics: “Once, I had an empire in a golden age” AND “And I feel like my castle’s crumbling down / And I watch all my bridges burn to the ground / And you don’t want to know me, I will just let you down / You don’t wanna know me now” AND “Once, I was the great hope for a dynasty / Crowds would hang on my words and they trusted me / Their faith was strong, but I pushed it too far / I held that grudge ’til it tore me apart // Power went to my head and I couldn’t stop / Ones I loved tried to help, so I ran them off / And here I sit alone behind walls of regret / Falling down like promises that I never kept” AND “People look at me like I’m a monster // Now they’re screaming at the palace front gates / Used to chant my name / Now they’re screaming that they hate me / Never wanted you to hate me”
8. There It Goes by Maisie Peters
I love this song so, so much. There’s something about the delicacy of the production and Maisie’s light voice and the uplifting feel that makes me emotional every time, not to mention the absolutely stunning lyrics. She seems to sum up the whole album in one song, moving forward and reclaiming her story, with more beautiful imagery than you know what to do with. The song has a lightness and a freedom to it, that we’re introduced to in the first part of the song, with lyrics like “I’m back in London / I’m running down Columbia Road / They’re selling sunflowers cheap” and “I hang all my art / And I dance with the coven / As the rain falls hard on the street,” resolving with “And I, I’m doing better / I made it to September / I can finally breathe,” a quiet but self-assured acknowledgement of how far she’s come. In the chorus, she’s finally letting go of this relationship that she’s invested so much time and emotion in; she’s letting it go before it becomes a permanent part of her. In the second verse, she’s moving forward and finally feeling like it: “I / Need you less than I did / I threw a party / He kissed me right in front of my friends / I felt so far from the cliffs.” She’s found peace with it and with what they had – “I sleep through the night / And I go where I’m wanted / And I don’t need your light to be lit” – and she’s taken from it what she needed to – “But oh, the way I loved you / I will not be embarrassed of that / Just should’ve known when to quit” – and nothing more. After the second chorus, she tips into an incredible bridge, full of symbolism and imagery, representing starting over and recovery: “A new home, a swan dive / A blank page, a rewrite / A black cat in the streetlights / An open door / The comedown of closure / The girls and I do yoga / I wake up and it’s October / The loss is yours / Brick lane in the brisk cold / And red wine on his hip bone / The witching hours of Stockholm that you won’t see / Sunflowers in the kitchen / No heartbreak in remission / The universe is shifting / And it’s all for me, all for me.” Her world has turned on its axis and the story has become hers again; she’s taken it back. The bridge always makes me cry. I want to know what that feels like, that “The universe is shifting / And it’s all for me” feeling. It’s a beautiful, beautiful song and one that has a really special place in my heart, even if it often makes me cry.
Favourite Lyrics: “I’m back in London / I’m running down Columbia Road / They’re selling sunflowers cheap” AND “I hang all my art / And I dance with the coven / As the rain falls hard on the street / And I, I’m doing better / I made it to September / I can finally breathe” AND “I sleep through the night / And I go where I’m wanted / And I don’t need your light to be lit / But oh, the way I loved you / I will not be embarrassed of that / Just should’ve known when to quit” AND “A new home, a swan dive / A blank page, a rewrite / A black cat in the streetlights / An open door / The comedown of closure / The girls and I do yoga / I wake up and it’s October / The loss is yours / Brick lane in the brisk cold / And red wine on his hip bone / The witching hours of Stockholm that you won’t see / Sunflowers in the kitchen / A heartbreak in remission / The universe is shifting / And it’s all for me, all for me”
Later on, in September, the line “I made it to September / I can finally breathe” became a bit of a trend on social media and people were screaming it during the live show. I struggled with that: I love the song and it just made me really sad because I didn’t feel good about reaching September, I wasn’t doing better, and I couldn’t ‘finally breathe.’ I want, more than anything, to know what “The universe is shifting / And it’s all for me” feels like. So seeing all of those videos was really hard and I ended up all but quitting social media. So it meant a lot to me when Maisie posted this clip…
9. making the bed by Olivia Rodrigo // logical by Olivia Rodrigo // the grudge by Olivia Rodrigo
I literally cannot choose so it’s a three-way tie between my three favourite songs from GUTS, Olivia Rodrigo’s new album.
‘making the bed’ is a gorgeous, gorgeous song while still being utterly devastating; the soft, delicate vocals and production only emphasise the vulnerability of the song. The song seems to detail Rodrigo’s experience of and feelings on fame but so many of the lyrics can also apply to feeling uncomfortable in your surroundings and in your skin, such as “Well, sometimes I feel like I don’t wanna be where I am” and “I’m so tired of bein’ the girl that I am.” The overthinking and feelings of insecurity are clear too, with lyrics like “Every good thing has turned into somethin’ I dread.” It’s very relatable, regardless of Rodrigo’s personal meaning. The metaphor she uses in the chorus, the idea of making her own bed is already a powerful one but, by expanding it, she’s made it even more impactful: “But it’s me who’s been makin’ the bed / Me who’s been makin’ the bed / Pull the sheets over my head, yeah / Makin’ the bed.” Not only has she created the situation she’s in but, now that she’s aware of it, it’s so hard to fix that she’s hiding from what she has to do, pulling the ‘sheets’ over her head. The second verse is one of my favourite lyrical moments on the album and I deeply relate to the part about the recurring dream: “And every night, I wake up from this one recurrin’ dream / Where I’m drivin’ through the city, and the brakes go out on me / I can’t stop at the red light, can’t swerve off the road / I read somewhere it’s ’cause my life feels so out of control / And I tell someone I love them just as a distraction / They tell me that they love me like I’m some tourist attraction / They’re changin’ my machinery, and I just let it happen / I got the things I wanted, it’s just not what I imagined.” It’s so beautifully written and the emotion just feels so raw and so close to the surface; it hits me like a train every time. It’s so vivid and visceral. The guitar part in the bridge is absolutely gorgeous and it may be my favourite musical moment on the album; there’s something about the tone combined with the melody that just hits me like a gut punch. I love it and it makes me want to flip my hair dramatically every time. And the last chorus is just so sad – “Sometimes I feel like I don’t wanna be where I am / Countin’ all of the beautiful things I regret / But it’s me who’s been makin’ the bed / Me who’s been makin’ the bed / Pull the sheets over my head / Makin’ the bed” – the modified lines adding one last heartbreaking confession.
Favourite Lyrics: “Another perfect moment that doesn’t feel like mine / Another thing I forced to be a sign” AND “I’m so tired of bein’ the girl that I am / Every good thing has turned into something I dread / And I’m playin’ the victim so well in my head / But it’s me who’s been making the bed / Me who’s been making the bed / Pull the sheets over my head / Making the bed” AND “And every night, I wake up from this one recurrin’ dream / Where I’m drivin’ through the city and the brakes go out on me / I can’t stop at the red light, I can’t swerve off the road / I read somewhere it’s ’cause my life feels so out of control / And I tell someone I love them just as a distraction / They tell me that they love me like I’m some tourist attraction / They’re changin’ my machinery and I just let it happen / I got the things I wanted, it’s just not what I imagined”
I think ‘logical’ may be the best written song on the album (and, interestingly, it’s a cowrite with Julia Michaels, which could explain the slightly different lyrical voice). The production is gorgeous – I love the piano part so much – and Rodrigo sounds beautiful: hurt and heartbroken and confused. Her vocals are incredible across the album but I think this song really showcases how expressive her voice can be. Lyrically, it’s stunning and I particularly love the second verse: “And I fell for you like water / Falls from the February sky / But now the current’s stronger / And I couldn’t get out if I tried / But you convinced me, baby / It was all in my mind.” The way she weaves all of these water based lyrics together so that they flow smoothly is beautiful. The simplicity of both the lyric and the melody of the chorus sounds stunning and really emphasises the vulnerability, as does the use of such… almost childish imagery: the lyrics “Two plus two equals five” and “If rain don’t pour and sun don’t shine” makes her sound so young, which she arguably was in the face of the break up. The bridge is incredible and so, so vulnerable (I’m honestly amazed that she released it): “‘Cause lovin’ you is lovin’ every / Argument you held over my head / Brought up the girls you could have instead / Said I was too young, I was too soft / Can’t take a joke, can’t get you off / Oh, why do I do this?” And it’s so well-written: you can hear his systematic and undermining attack on her, hammering on every insecurity and soft spot. You can hear the cruelty and you can hear her anguish and humiliation. And as heartbreaking as that is, it’s the outro, I think, that reveals the core of the pain: “Oh, logical, logical, love is never logical / I know I’m half responsible and that makes me feel horrible / Oh, logical, logical, love is never logical / I know I could’ve stopped it all, God, why didn’t I stop it all?” The first part hits like a gut punch and the second part is worse; it’s gut-wrenching to listen to. To hear her question why she let it happen, why she didn’t stop it before it got to that point, when he was the one who hurt her is devastating. But I get it; I’ve been there and something like that really messes with your head, making it really, really hard to untangle the feelings from the facts.
Favourite Lyrics: “Come for me like a saviour / And I’d put myself through hell for you” AND “And I fell for you like water / Falls from the February sky / But now the current’s stronger / No, I couldn’t get out if I tried
But you convinced me, baby / It was all in my mind” AND “Then changing you is possible / No, love is never logical” AND “You built a giant castle / With walls so high I couldn’t see / The way it all unraveled / And all the things you did to me / You lied, you lied, you lied” AND “You mean all those words you said / I’m sure that girl is really your friend / Problems are all solvable / ‘Cause loving you is loving every // Argument you held over my head / Brought up the girls you could have instead / Said I was too young, I was too soft / Can’t take a joke, can’t get you off” AND “Logical, logical / Love is never logical / I know I’m half responsible / And that makes me feel horrible // Oh, logical, logical / Love is never logical / I know I could’ve stopped it all / God, why didn’t I stop it all?”
‘the grudge’ is an interesting one; it feels a little more stream of consciousness than traditional pop song. The chords wander a little more and it’s not so tightly tied up. But it’s beautiful and raw, a plea for answers after a trauma that changed your life in every possible way imaginable. I really relate to that and so I find the lyrics deeply moving and compelling; I can pinpoint lyrics like “You took everything I loved and crushed it in between your fingers” and “And I doubt you ever think about the damage that you did / But I hold on to every detail like my life depends on it / My undying love, now I hold it like a grudge” to moments in my own life. While I prefer the verses more from a lyrical point of view, the chords to the chorus are gorgeous, especially towards the end of the first chorus: she makes a transition that is just so gorgeous and vividly reminds me of Sara Bareilles, or something Sara Bareilles would do in a song. It’s one of my favourite musical moments on the album. And the second verse is another of my favourite lyrical moments: “The arguments that I have won against you in my head / In the shower, in the car and in the mirror before bed / Yeah, I’m so tough when I’m alone and I make you feel so guilty / And I fantasise about a time you’re a little fucking sorry / And I try to understand why you would do this all to me / You must be insecure, you must be so unhappy / And I know in my heart hurt people hurt people / And we both drew blood, but, man, those cuts were never equal.” Each moment is so clear, so vivid: you can see each imagined argument, her frustration and distress over how she never got the apology she deserved, how hard she’s trying to let it go only to still feel so hurt by it. No word is superfluous; every syllable is dedicated to this attempt to exorcise him from her life – to let it go, to forgive him, to move on – but she’s still hurting too much. Her vocals in the bridge are stunning and when it peaks, with the lyric “You have everything and you still want more,” you can almost hear the tears. That feeling, that pain and frustration and anger, is conveyed so well that it makes my stomach twist. The progression within the chorus, from “It takes strength to forgive, but I don’t feel strong” to “It takes strength to forgive, but I’m not quite sure I’m there yet,” really show the growth and acceptance throughout the song: at the beginning, she’s frustrated with herself for not being able to forgive him but, by the final chorus, she’s accepted that it’s a process and a journey and she’ll get there one day, but she’s just not in that place ‘yet.’ It’s acknowledgement that it’s okay to feel everything, to process it all in small steps; she doesn’t have to be anywhere she isn’t until she’s ready to be. Maybe that’s just me reading into it but I think it’s a really moving sentiment.
Favourite Lyrics: “Took everything I loved and crushed it in between your fingers / And I doubt you ever think about the damage that you did / But I hold onto every detail like my life depends on it” AND “The arguments that I have won against you in my head / In the shower, in the car and in the mirror before bed / Yeah, I’m so tough when I’m alone and I make you feel so guilty / And I fantasise about a time you’re a little fuckin’ sorry / And I try to understand why you would do this all to me / You must be insecure, you must be so unhappy / And I know in my heart hurt people hurt people / And we both drew blood, but, man, those cuts were never equal” AND “You have everything and you still want more” AND “It takes strength to forgive, but I’m not quite sure I’m there yet”
10. The Tree by Maren Morris // Truth Is by Maisie Peters // Say Don’t Go (Taylor’s Version) [From The Vault] by Taylor Swift
I love both of the tracks on Maren Morris’ EP, The Bridge, but I had to go with ‘The Tree’ here. I just really, really love it. She sounds incredible, as she always does, and the production is gorgeous; it just sounds so Maren Morris in all of the best ways. The chorus – “Oooh / Do you hear that / It’s the sound of a new wind blowing / Oooh / Do you feel that / Heart letting go of the weight it’s been holding / I’ve made miracles in the shadows / But now that I’m out in the sun / I’ll never stop growing / Wherever I’m going / Hope I’m not the only one” – is so moving and inspiring. The tree metaphor is really tight and beautifully executed and the lyrics are so simple but impactful: “I’m done filling a cup with a hole in the bottom / I’m taking an axe to the tree / The rot at the roots is the root of the problem / But you wanna blame it on me” and “I hung around longer than anyone should / You’ve broken my heart more than anyone could” and “Spent ten thousand hours trying to fight it with flowers.” And the extended final chorus, with the added lyrics – including “Do you hear that / That’s the sound of the tree falling” – is the perfect ending. The song expresses her feelings and her hopes, but it’s also a call to action. Over her career, Maren has become more and more outspoken about her personal and political beliefs and this seems like a really natural progression. It’s really powerful, even if it does make me want to cry and give her a massive hug.
Favourite Lyrics: “The rot at the roots is the root of the problem / But you wanna blame it on me / I hung around longer than anyone should / You’ve broken my heart more than anyone could” AND “Ooh, do you hear that? / It’s the sound of a new wind blowing / Ooh, do you feel that / Heart letting go of the weight it’s been holding / I’ve made miracles in the shadows / But now that I’m out in the sun / I’ll never stop growing / Wherever I’m going / Hope I’m not the only one” AND “Spent ten thousand hours trying to fight it with flowers” AND “Do you hear that / That’s the sound of the tree falling”
I love The Good Witch deluxe tracks. I love the original album and I wouldn’t change the tracklist because it’s so perfect as it is but I still love the extra songs. There are so many gorgeous lyrics and melodies and production moments. There are multiple songs I could write about here but the one that hit me the hardest and fastest was ‘Truth Is.’ It’s just so raw and devastating and it breaks my heart to think of Maisie writing it, of Maisie potentially going through it – she’s said that she doesn’t only write about personal experiences so I don’t want to assume that she has but it’s clearly a story that resonated with her otherwise I doubt she would’ve written a song about it, and such a powerful song at that – having said that, I will refer to ‘she/her’ and ‘he/him’ just for the sake of ease while writing. It describes, in painful detail, reflecting on an abusive relationship and the devastating effect it had. The lyrics just wrecked me, the trauma she went through and how he clearly just doesn’t care: “Time will heal / But I’ll always be a little bit broke.” I love the metaphor and imagery in the lyric “Hey baby, all I ever did was care / You played a bitter game of musical chairs” and this revelatory moment – “I was a failure ’til I couldn’t fuckin’ bear it no more” – is so heartbreaking and a feeling that I do really relate to. In the bridge, the ways she questions why he did what he did – “Did I rile up all your demons? / Did I give you any reason? / Or did I love you? Did I just love you? / Was it useful? Was it worth it? / Did you think that I deserved it? / ‘Cause I didn’t, I just loved you” – is so relatable, for anyone who’s been treated badly by someone. There’s self-blame – “Did I rile up all your demons? / Did I give you any reason?” – and trying to make sense of why – “Was it useful? Was it worth it? / Did you think that I deserved it?” – but ultimately, she knows that she didn’t do anything wrong: “‘Cause I didn’t, I just loved you.” The choruses are so powerful but it’s the final one that really ripped my heart out: “Truth is, you were the blow behind the bruises / You weren’t love and if I could undo it / I’d never have been yours to ruin / You got off with no court and no blame / Who is out there living with no shame? / Who took my very worst fear and proved it? / Truth is, you did.” There’s the desperation to rewrite the past and the pain of being “yours to ruin,” implying that she feels ruined (which goes back to “I’ll always be a little bit broke”); the fact that he “got off with no court and no blame” and that he’s “living with no shame” conjures a very specific scenario that just makes me want to cry, an image that he isn’t weighed down by this while she is; and the idea that he “proved” her “worst fear” is such a distressing one. It’s such a powerful and moving song and it will always be special because of how raw the emotion is; my experiences don’t line up exactly but there are a lot of parallel emotions, enough that I could certainly sing lines of this song to a certain person who damaged me.
Favourite Lyrics: “And that’s real / But it doesn’t stop the lump in my throat / Time will heal / But I’ll always be a little bit broke” AND “Still you believe there’s no wound and no blood / Who took all of my trust then abused it? / Truth is, you did” AND “Hey baby, all I ever did was care / You played a bitter game of musical chairs / Hey baby, I would fall and you would glare / I was a failure ’til I couldn’t fuckin’ bear it no more” AND “And I’ll never get back months of my life / Time will cure / But you’re never gonna know what that’s like” AND “Did I rile up all your demons? / Did I give you any reason? / Or did I love you? Did I just love you? / Was it useful? Was it worth it? / Did you think that I deserved it? / ‘Cause I didn’t, I just loved you” AND “Truth is, you were the blow behind the bruises / You weren’t love and if I could undo it / I’d never have been yours to ruin / You got off with no court and no blame / Who is out there living with no shame? / Who took my very worst fear and proved it? / Truth is, you did”
I was so excited for the vault tracks of 1989 and they did not disappoint; they’re great songs and I honestly love them all (although I can absolutely see why they weren’t included on the original tracklist). Picking just one for this month, especially since the album only came out on the 27th, was really hard but the atmospheric ‘Say Don’t Go’ (Taylor’s Version) [From The Vault] was a favourite from my first listen. I love the dark, atmospheric sound that’s still very much 1989 and Taylor’s vocals are stunning, as are the backing vocals (which also feel very 1989). The lyrics are gorgeous. I love the opening line: “I’ve known it from the very start / We’re a shot in the darkest dark / Oh no, oh no, I’m unarmed.” It feels like such a perfect opening to the song and I love the imagery throughout the verse lyrics: “Now I’m pacin’ on shaky ground / Strike a match, then you blow it out / Oh no, oh no, it’s not fair” really reflects the uncertainty and anxiety she felt about the relationship and “‘Cause you kiss me and it stops time / And I’m yours, but you’re not mine / Oh no, oh no, you’re not there” is so visceral and heartbreaking. The refrain, “Say, ‘Don’t go’ / I would stay forever if you say, ‘Don’t go,'” is simple but the emotion in her voice is so moving. I love the way the melody rises into the chorus and it’s so catchy: “Why’d you have to lead me on? / Why’d you have to twist the knife? / Walk away and leave me bleedin’, bleedin’? / Why’d you whisper in the dark? / Just to leave me in the night? / Now your silence has me screamin’, screamin’ / (Say) say, ‘(don’t) don’t (go) go’ / I would stay forever if you (say) say, ‘(don’t) don’t (go) go.'” It feels deeply cohesive to the sounds and styles and themes of the original album but more intense maybe, more vulnerable. I wonder if that is why it didn’t make the original tracklist. The bridge is plaintive and heartbroken – “Why’d you have to / Make me want you? / Why’d you have to / Give me nothin’ back? / Why’d you have to / Make me love you? / I said, ‘I love you’ / You say nothin’ back” – and is deeply reminiscent of ‘You’re Losing Me’ (or the other way around, given that the former was written first). It’s so cool to see how many links there are both to repeated themes on throughout the album – to madness, to fire, to darkness – and to specific songs – to driving by, like in ‘I Wish You Would,’ and card games, like in ‘New Romantics’ – something that makes Taylor’s writing so interesting. 1989 is one of the albums where it’s most striking so it’s fascinating to see that she clearly employed it as a technique throughout the songwriting process for the album; otherwise we wouldn’t be seeing it in the songs that didn’t make the original album.
Favourite Lyrics: “I’ve known it from the very start / We’re a shot in the darkest dark / Oh no, oh no, I’m unarmed” AND “I’m standin’ on a tightrope alone / I hold my breath a little bit longer” AND “Now I’m pacin’ on shaky ground / Strike a match, then you blow it out / Oh no, oh no, it’s not fair / ‘Cause you kiss me and it stops time / And I’m yours, but you’re not mine / Oh no, oh no, you’re not there” AND “Why’d you have to / Make me want you? / Why’d you have to / Give me nothin’ back? / Why’d you have to / Make me love you? / I said, ‘I love you’ / You say nothin’ back” AND “I would stay forever if you say, ‘Don’t go’ / But you won’t, but you won’t, but you won’t”
11. The Last One by Maisie Peters
I was lucky enough to see Maisie twice on The Good Witch Tour, first on Halloween in Bristol and then at Wembley Arena (her first arena as a headliner!) at the beginning of November. Both shows were really special and so I had to choose this song for my November slot since she dedicated it to fans every time she performed it live. When she posted the video of the Wembley show, she used this song and the accompanying message read: “wembley was a perfect show and a perfect night, a true celebration of the good witch and the magic that has brought us all together. this song to me has always been about you guys, about how we feel about eachother, about how safe and special and sacred our shows are, so i knew straight away the video had to showcase that. i hope u feel seen and heard and understood, and truly reminded of how much love there is and always will be in this universe we have created together.” It’s a gorgeous song, triumphant and uplifting, and I love it so much. The song sees Maisie describing someone she loves, regardless of their mistakes and failures, and how she’ll always support him. In the first verse, she likens him to Icarus: “You’re bright and it’s blinding / Just a small spark, and you’re flying / With your wax wings in a back room / Got my arms out, tryna catch you.” And while many might consider him “a lost cause in Levi’s,” she’ll “always see great heights” in him. In the chorus, she establishes just how much she’ll support him, that she’ll be the last one beside him if that’s what it comes to: “I’ll be the last one / I’ll be the last one in your corner when the count’s done / I’ll be the last one / Holdin’ my hands up / Stood on the bleachers all alone after the crowd’s gone / I’ll be the last one.” In the post-chorus, the energy and imagery kicks up in intensity with lyrics like “If you’re the Syd Barrett of the band, I’m the girl on the train tracks holdin’ your hand.” I love that lyric in particular. I’ve seen the interpretation that it’s about how, even if he’s lost everything, she’ll still follow him and be there to hold his hand; Syd Barrett being used as a symbol of loss – lost dreams, lost youth, lost idealism – and the train tracks potentially referring to a quote about his reclusiveness (“Syd didn’t so much ‘get off the train’ as fall headlong onto the tracks”). It’s a heartbreaking lyric. She continues with the use of gorgeously vivid imagery in the second verse and bridge, such as “You’re a dreamer in a parka / Send a flare up in the dark / And I’ll come find ya” and “When all the floodlights blow / And the sky is filled with smoke.” The final chorus begins as a breakdown chorus, gentle and tender, before bursting back into life to end the song, with modified lyrics in the post-chorus: “‘Cause, if you’re the Syd Barrett of the band / I’m the girl on the train tracks holdin’ your hand / Halfway to the moon on a plane you couldn’t land / You were seeing castles, they were seeing sand / They’re never gonna get it, no, they’ll never understand / But I believe in you, I’m your number one fan / So, after the crowd’s gone / I’ll be the last one.” I love the childish naïvety in the lyric “You were seeing castles, they were seeing sand,” like he can still appreciate the moments of beautiful simplicity while everyone else doesn’t even notice them. It’s very sweet. The song displays such a tender love for the person it’s about, such belief in them, making it really moving. Musically, I love the anthemic sound – the arrangement and production are gorgeous – and I love the little added effects, like the sound of the flare alongside the “Send a flare up in the dark” lyric. Maisie’s voice sounds incredible and the atmospheric backing vocals are just so perfect. With all of the elements of the song combined, plus Maisie’s continued sincere dedications of the song, just makes me so emotional; I’ve cried while listening to it more than once.
Favourite Lyrics: “You’re bright and it’s blinding / Just a small spark, and you’re flying / With your wax wings in a back room / Got my arms out, tryna catch you” AND “Caught in a streetlight / A lost cause in Levi’s / But I’ll always see great heights in you” AND “I’ll be the last one / I’ll be the last one in your corner when the count’s done / I’ll be the last one / Holdin’ my hands up / Stood on the bleachers all alone after the crowd’s gone / I’ll be the last one” AND “If you’re the Syd Barrett of the band, I’m the girl on the train tracks holdin’ your hand” AND “But I’ll believe in you, still your number one fan, baby / After the crowd’s gone, I’ll be the last one” AND “You’re a dreamer in a parka / Send a flare up in the dark / And I’ll come find ya / Somewhere downtown / With your worst friends on the last round” AND “When all the floodlights blow / And the sky is filled with smoke / You’re still out there on your own / And I’m still the last to go” AND “You were seeing castles, they were seeing sand / They’re never gonna get it, no, they’ll never understand”
12. Is It Over Now? (Taylor’s Version) [From The Vault] by Taylor Swift
This song is another example of how great the 1989 vault tracks are. The vocals, the backing vocals, the imagery, the energy, the production… they’re all gorgeous. As a song, it fits into the story Taylor is telling on 1989 – it’s practically a summation of the whole relationship – but given how desperate Taylor was to protect both Harry Styles and her reputation, it’s not surprising that it didn’t end up on the final tracklist; the album was marketed heavily as her ‘single girl album’ and she worked so hard to avoid the album becoming thought of as another heartbreak album so a song like this, especially with its similarities to ‘Out of the Woods,’ may well have tipped the delicate balance she was clinging to. The lyrics are full of uncertainty and frustration as she tries to make sense of the breakup. She still sees him everywhere – “Let’s fast forward to three hundred takeout coffees later / I see your profile and your smile on unsuspecting waiters” – and clearly thinks that he feels the same, that he can’t get over her either – “You dream of my mouth before it called you a lying traitor” – despite how things ended and that he’s using his new relationships to try and find what they had – “You search in every maiden’s bed for something greater.” And when she repeats this lyric later in the song, the situation has evolved – “You search in every model’s bed for something greater” – and he’s moved from maidens to models, which most likely implies that, with more time and more fame, he dated more and more beautiful women, women as opposed to girls and beautiful because they had to be for their job but that he’s still looking for someone ‘better’ than Taylor and not finding it (an interesting link to these lyrics can be found in ‘Wonderland,’ with the lyric “You searched the world to something else to make you feel like what we had”). The chorus seems to ask when the relationship was truly over, although whether she’s asking about it in the literal or emotional sense, we can’t know: “Baby, was it over / When she laid down on your couch? / Was it over when he unbuttoned my blouse? / ‘Come here,’ I whispered in your ear / In your dream as you passed out, baby / Was it over then? / And is it over now?” Both options are really interesting to think about, both in how to interpret the song and how each potentially changes the story that the album tells. The second verse details moments that we know featured in their relationship: “When you lost control / Red blood, white snow” clearly refers to their snowmobile accident that she wrote about in ‘Out of the Woods’; “Blue dress on a boat” seems likely to reference the day they went out on a boat together, which the paparazzi reported with a photo of her sitting alone on the back of said boat; and “Your new girl is my clone” is likely a comment on the women he later dated who looked very like Taylor, as is “Let’s fast forward to three hundred awkward blind dates later / If she’s got blue eyes, I will surmise that you’ll probably date her,” which is a beautifully scathing lyric. This song plays with structure, bringing in the bridge before the second chorus, and she describes the hurt she feels watching him flaunt his new relationships when she’s been respecting his feelings by keeping hers private: “And did you think I didn’t see you? / There were flashing lights / At least I had the decency / To keep my nights out of sight / Only rumors ’bout my hips and thighs / And my whispered sighs / Oh, Lord, I think about / Jumping off of very tall somethings / Just to see you come running / And say the one thing I’ve been wanting / But no.” The melodic rhythms and internal rhymes are super satisfying and really increase the pace of the section. I struggle with the last part though: “I think about / Jumping off of very tall somethings / Just to see you come running / And say the one thing I’ve been wanting.” I know what she means – she’s using the metaphor to describe how extreme her feelings are, how far she’d go to have him come back – but I can never be okay with such a casual use of suicidal imagery, like “Jumping off of very tall somethings,” especially when it’s used in the context of getting someone’s attention. It’s something like this that means a song can never rise as high on personal ranking as it could have without such a lyric. After that bridge, she jumps in to the second pre-chorus and chorus before returning to the bridge and, from there, a messy and therefore highly representative outro that pulls lyrics from multiple sections of the song. Despite the anxiety and distress in the song, it’s super catchy and fun, and it’s easy to find yourself listening to it on a loop. The writing is so, so good and it’s songs like this one that really show us how she grew as a songwriter from this album to reputation.
Favourite Lyrics: “Was it over then? / And is it over now?” AND “When you lost control / Red blood, white snow / Blue dress on a boat / Your new girl is my clone” AND “And did you think I didn’t see you? / There were flashing lights / At least I had the decency / To keep my nights out of sight / Only rumours ’bout my hips and thighs / And my whispered sighs / Oh, Lord” AND “Let’s fast forward to three hundred awkward blind dates later / If she’s got blue eyes, I will surmise that you’ll probably date her”
One day, I’ll actually keep to the twelve songs a year and we’ll all faint in shock, myself included. But that is not this year. When there’s so much good music in the world, I’m not surprised I can’t keep to it but it is kind of fun and motivating to try, to attempt to determine the songs that have had the biggest impact on me in any given month. As usual, it’s gotten very long so, if you’ve made it this far, thank you very much. I hope you found a song or two that you liked, an artist that you want to hear more of. Again, here’s the playlist if you want to listen to any (or all) of the songs again.
Category: about me, anxiety, autism, depression, emotions, favourites, medication, mental health, music, quotes, special interests, suicide, video, writing Tagged: 1989, 1989 taylor's version, actuallyautistic, antidepressants, autism, autistic, autistic adult, autistic artist, autistic creative, candi carpenter, castles crumbling, crashlanded, depression, favourite songs, from the vault, guts, hayley williams, history of man, ingrid andress, is it over now, kelsea ballerini, let it be love, logical, lost the breakup, lyrics, madeline edwards, maisie peters, making the bed, maren morris, medication, melodies, melody, mental health, mental illness, michael logen, mountain with a view, music, nashville, nervous system, nick wilson, olivia rodrigo, phenelzine, production, rolling up the welcome mat, sara bareilles, say don't go, she used to be mine, song analysis, songs, songs of 2023, songwriting, speak now taylor's version, special interest, special interests, subject to change, taylor swift, the good witch, the good witch deluxe, the last one, the six one five collective, the tree, there it goes, tin pan south, tin pan south 2023, truth is, you're losing me
Changing Therapist
Posted on November 5, 2023
TW: Mentions of self harm and suicidal thoughts and urges.
It’s been a year since I started therapy again after an unintentional break, essentially starting again with a new therapist. It’s been a hard and emotional process, and at times a distressing one; just going to therapy can make you feel so vulnerable and so open to further hurt as you dig into the hard stuff – wading into dark waters that you’d rather ignore and pretend don’t exist, even as they’re eroding your mental health – that adding difficulties to that already difficult thing can feel unfairly cruel. So, given that I’m me, I thought that, perhaps, writing about it might be helpful and maybe not just for me but for anyone going through a similar transition. And if not helpful, then hopefully validating in some way.
I’d been seeing Therapist A for almost seven years when everything changed. She was taking leave and I was on my own.
Pre-2021, I’d seen Therapist A once or twice a week pretty consistently since early 2016. Even when the UK went into lockdown due to COVID-19 at the beginning of 2020, we continued our sessions online; I didn’t find them as productive but it was better than nothing. We continued that way for a while, trying to manage my crippling anxiety over the pandemic, working on issues that came up as I persisted with my now online Masters classes, and continuing to work on the issues that had landed me in therapy in the first place. But then the schedule began to slip: Therapist A’s home life was pulling her away from work and I was working myself into the ground in order to complete the final project of my Masters. I barely saw her in the last four months of the course, which I really struggled with: I was digging into some pretty hard stuff, writing song after song about my experience of being autistic, and I craved that safe space to play them to her, to hear her perspective on what I was saying, talk about the feelings they were bringing up, and she wasn’t there. I told myself that it was a short term thing and that, once the Masters was over and her stuff was resolved, the schedule of our sessions would go back to normal. I think it’s safe to say that, given the title of this post, it didn’t.
I finished the Masters in September 2021 and officially graduated, walking the stage, a few months later in November. I had reduced and stopped taking Phenelzine at this point, in preparation for trying ADHD meds (and we all know how appallingly that went), and my depression was creeping back in; the situation was getting pretty desperate. But luckily, that was when Therapist A reached out and we started having sessions again. We had a lot of catching up to do but, by mid-December, we were up to date. Unfortunately, the ADHD medication was already hitting me hard and my depression had gone from a state I recognised to a whole new level of despair with increasingly overwhelming suicidal thoughts. My most vivid memory from that time is sitting in Therapist A’s new office, staring at the unfamiliar rug and hearing my voice in my ears as I confessed to those thoughts, my voice completely flat (this is known as ‘flat affect,’ a recognised symptom of depression and other mental health conditions). It still makes me nauseous to think about, even though so much time has passed and my depression has gotten so much worse since; I think, in my head, that was the beginning of this awful, awful time.
My last session was on New Years Eve and I was drowning, all of the impending new beginnings feeling more like a threat than a promise. When we hung up, I felt achingly hollow and that was only the beginning of a terrible night. But that’s a story for another time. January was passing around me, aimless and anxious, when I finally heard from Therapist A. But instead of setting up our next session, she was letting me know that she was taking leave indefinitely. Her reasons aren’t mine to tell but, between those, my ongoing abandonment issues, and my overwhelmingly bad mental health, I was devastated, spiralling into some grotesque hybrid of a meltdown and a panic attack that went on for hours: I screamed, I cried, I scratched at my face, I tore at my hair, I shrieked like an animal in pain. I guess that’s what I was. I felt like I was trying to exorcise a corrosive demon from my body but nothing helped, nothing alleviated the pain. I was shattered as brutally as if I’d been hit by a wrecking ball. That’s what it felt like, what my life felt like.
Eventually I physically ran out of energy and fell asleep, too tired and emotionally drained to even engage with the world. My depression became more and more overwhelming, compounded by the devastating effects of the ADHD medications and the loss of a massive source of support in my life, and, for months afterwards, I barely got out of bed, barely ate, barely talked. I abandoned social media and I avoided mirrors at every opportunity, to the point where I started to forget what I looked like. The suicidal thoughts were only getting stronger, stronger than they’d ever been in my life, and the feeling of being intrinsically, irreparably broken was – and is – a constant weight in my chest.
I’m not sure when or why I started getting out of bed, why I decided that I needed to go back to therapy. I think I knew I was getting into a very precarious position mentally and the excruciating pain of being inside my head was getting so unbearable that I was willing to do anything to lessen the pressure. I did see a consultant at the local mental health unit but the experience was another traumatic one: after a panic attack at the front door, a junior doctor took my history and then brought in the consultant who told me about ECT and the Ketamine trials before telling me why I shouldn’t do them and recommending doing more of the things I love (which I’d already told him I couldn’t engage with because I was so depressed). So that didn’t improve my relationship with doctors and the medical profession.
For a short while, I worked with a therapist I’d met several years previously but the sessions only made me feel worse and while I have no doubt that it wasn’t intentional, I ended up feeling more broken and more traumatised by some of the things he said, trauma that I’m still carrying around with me. So I stopped seeing him and met with several new therapists, trying to get a feel for them and their methods before committing to someone new. But, just like with Therapist A, Therapist B was the first of the group that I met (a year ago yesterday, I believe) and between her therapeutic approach, her personality, and the fact that she’d brought along a dog she knew in order to put me at ease, she was the obvious choice.
As therapists, they both trained in several of the same disciplines and their skillsets overlap to a certain degree but, when discussing a particular issue, there were differences to how they’d approach it; there has been a fair amount of whiplash in getting use to Therapist B’s approach after so many years with Therapist A. But the point of this post isn’t to compare them – they’re both lovely people and very good at what they do, at least as far as I can tell – but rather to reflect on the process of moving from one to another and the feelings that that kicked up. And a lot of feelings there were – I even wrote a song about it called ‘Grave Digger.’ During the early sessions with Therapist B, we made a timeline of my life and discussed some of the biggest moments, many of which were difficult and distressing (and remain so to this day). Revisiting and recounting the hardest parts of my life was gruelling but I did my best to push through the internal resistance and breathe through the resulting turmoil; between that and the ongoing mental anguish, it was a difficult few months. I don’t mean to make it sound like one continuous torture because that isn’t true -we’ve talked about the good experiences that’ve made me who I am, of course, and there have been sessions where we’ve laughed a lot – but I think that building a strong relationship with a therapist and making progress will always involve periods of incredible vulnerability, which is always scary and, at times, painful.
Sometimes – okay, often – I feel like I’m not making any progress at all, partly because of all the disruption and the distress it’s caused. A year ago, I hadn’t expected to see 2023 and my depression and chronic suicidal thoughts haven’t lessened, even though I am taking Phenelzine again (at a higher dose, in fact) – after many discussions with Therapist B. It has made me more functional, to a certain degree, but the decision came with a price tag: my self harming escalated from cutting my arm to cutting my face. I’m not convinced anything’s changed; I don’t feel any better. But I can see that some things have changed and changed for the better, even though I can’t feel the effects yet: something has allowed me to start talking about some of the worst stuff in my brain, even if only a little. It’s something I could never have imagined doing so I know that that’s progress, even though I struggle to feel it.
I have heard from Therapist A several times now; the news has generally been positive, which has been a great relief (and I appreciate having a little less uncertainty in my life). Therapy is continuing as normal – the current version of normal at least – which I’m pretty sure is a good thing: the idea of trying to work my way through all of the emotions that I know would come up as a result of any potential change makes me feel physically nauseous.
I’m not always convinced that I’ve adjusted and sometimes I forget that I’m not going to see Therapist A, my body moving in the direction of that office as the car turns down a different road; that experience is more ingrained than I had realised at the time. And I know I’m still carrying a lot of hurt and anger over the whole thing, even though over a year has passed. I’m not angry at the people involved – nobody chose any of this – but there is anger and, although I’ve been slower to realise it, hurt too. I think it’s easier to be angry than to be hurt. Not always but sometimes. And, as I said, I have abandonment issues, issues that I’ve struggled with for a long time, which – unsurprisingly – have been exacerbated by this whole thing. It’s hard to lose someone that you trusted to never leave (a naïve ideal, I know) and it’s hard to trust someone new, ignoring the whispers that they’re just another person who will inevitably walk away. I think these issues are important to mention but they probably need their own blog post rather than taking up space here: when talking about changing therapists, it’s not something that everyone has mixed into the equation. All of that said, I’m trying to trust and I think that, for the most part, I am, even if it does sometimes feel like a conscious, concentrated effort. The progress isn’t as fast as I’d hoped it would be when I committed to therapy again last year but the proof is there. I’m sharing things I never thought I’d share and that’s certainly not nothing.
Category: about me, anxiety, autism, covid-19 pandemic, depression, emotions, medication, meltdowns, mental health, self harm, suicide, therapy, treatment, university, writing Tagged: abandonment, abandonment issues, actuallyautistic, adhd, adhd medication, antidepressants, asc, asd, attention deficit hyperactivity disorder, autism, autism spectrum condition, autism spectrum disorder, autistic, autistic adult, autistic artist, autistic meltdown, autistic songwriter, covid, covid-19, cptsd, dbt, depression, dialectical behaviour therapy, ect, electroconvulsive therapy, fear of abandonment, flat affect, graduation, ketamine, ketamine trials, masters, masters degree, masters degree in songwriting, medical trauma, medication, meltdown, mental illness, online therapy, panic attack, phenelzine, radically open dialectical behaviour therapy, rodbt, self harm, self injury, songwriter, songwriting, suicidal, suicidal ideation, suicidal thoughts, suicidal urges, therapist, therapy, trauma, trd, treatment resistant depression, university

About Me
Hi! I’m Lauren Alex Hooper. Welcome to my little blog! I write about living with Autism Spectrum Disorder (ASD), ADHD (Inattentive Type), and Hypermobile Ehlers-Danlos Syndrome (hEDS), as well as several mental health issues.
I’m a singer-songwriter (it’s my biggest special interest and I have both a BA and MA in songwriting) so I’ll probably write a bit about that too.
My first single, ‘Invisible,’ is on all platforms, with all proceeds going to Young Minds.
My debut EP, Honest, is available on all platforms, with a limited physical run at Resident Music in Brighton.
I’m currently working on an album about my experiences as an autistic woman.
Links
Categories
Recent Posts
Archives
- May 2024 (1)
- April 2024 (3)
- March 2024 (1)
- January 2024 (1)
- December 2023 (4)
- November 2023 (6)
- October 2023 (5)
- September 2023 (6)
- August 2023 (4)
- July 2023 (5)
- June 2023 (5)
- May 2023 (7)
- April 2023 (4)
- December 2022 (4)
- November 2022 (1)
- October 2022 (1)
- September 2022 (1)
- August 2022 (3)
- June 2022 (2)
- May 2022 (6)
- April 2022 (10)
- March 2022 (9)
- February 2022 (3)
- January 2022 (1)
- December 2021 (7)
- November 2021 (5)
- October 2021 (7)
- September 2021 (4)
- August 2021 (1)
- July 2021 (2)
- June 2021 (4)
- May 2021 (10)
- April 2021 (11)
- March 2021 (14)
- February 2021 (6)
- January 2021 (6)
- December 2020 (8)
- November 2020 (9)
- October 2020 (8)
- September 2020 (10)
- August 2020 (8)
- July 2020 (4)
- June 2020 (6)
- May 2020 (8)
- April 2020 (7)
- March 2020 (9)
- February 2020 (5)
- January 2020 (7)
- December 2019 (7)
- November 2019 (1)
- October 2019 (1)
- August 2019 (1)
- July 2019 (2)
- June 2019 (3)
- May 2019 (5)
- April 2019 (5)
- March 2019 (5)
- February 2019 (6)
- January 2019 (5)
- December 2018 (7)
- November 2018 (3)
- October 2018 (5)
- September 2018 (5)
- August 2018 (5)
- July 2018 (9)
- June 2018 (7)
- May 2018 (7)
- April 2018 (6)
- March 2018 (11)
- February 2018 (5)
- January 2018 (6)
- December 2017 (7)
- November 2017 (7)
- October 2017 (7)
- September 2017 (6)
- August 2017 (5)
 Finding Hope
Finding Hope