2023 in Review
Posted on January 1, 2024
TW: Discussion of depression, self harm, and suicidal thoughts and ideation.
Much like last year, I have no idea how to sum up this year. I don’t think I have it in me to write a long post that involves such intense emotions and I think that, if I wait until I do, we might all be waiting a very long time so I’m just going to write until I can’t anymore and that’ll be that. It’s just too hard.
While there have been good moments (some of which can be seen in the collage below), it’s been a fucking painful year and it’s now the third New Year’s Eve that I’ve spent crippled by depression, suicidal thoughts, and overwhelming fear and dread around the future. I’m pretty sure I’m in full autistic burnout and I feel like I’m living in a fog. Last year, I think I described my depression as a drought but, this year, I think the better metaphor is drowning: I feel like I’m drowning in this depression and I have so little energy left that staying afloat is feeling more and more impossible. I’m so tired. I’m tired of trying so hard, of feeling like I’m not trying hard enough; I’m tired of feeling this way, of feeling like things will never get better, like there’s no point in even trying to feel better because there’s nothing worth feeling better for. It just feels like there’s so much bad in the world, so much agony, that it isn’t a world I want to live in. I feel broken; I feel like a prime example of a defective human being. There have been good things, like I said, but it seems like they can never just be good things: there’s always so much bad or hard twisted up in them that enjoying them isn’t as straightforward as it sounds. I miss feeling safe. I miss feeling safe to feel things.
A big, hard part of this year has been that I started taking Phenelzine again, for the third time. I didn’t want to and I felt coerced by the circumstances to take it. I was so angry about it all that I made potentially my most dramatic, self destructive move so far: I cut my face and then, when it got infected, I was so reluctant to treat it that I’ve ended up with a fairly visible scar. The most confusing part of it was that, even though I didn’t want anyone to bring it up, I was surprised that no one did; it seemed like the kind of thing that would trigger some alarm. Just as I imagined voicing consistent suicidal would but no one’s really commented on that either. It only makes the experience more isolating and lonely. But back to the Phenelzine: while it helped me get out of bed and go out now and then, it hasn’t had the same impact that it’s previously had on my mood, even on the higher dose. And that means that I’ve officially run out of medication options. I’ve been going to therapy consistently, for the most part, but I feel like it’s getting harder and harder; there have been sessions where I’ve left feeling traumatised. We’ll be trying something different in the new year but I’m struggling to feel hopeful, but that’s not specific to just therapy.
I look at the collage I made for this year and although I remember each of these moments, I feel disconnected from them; the emotions feel dulled. A lot has happened, somewhat to my surprise…
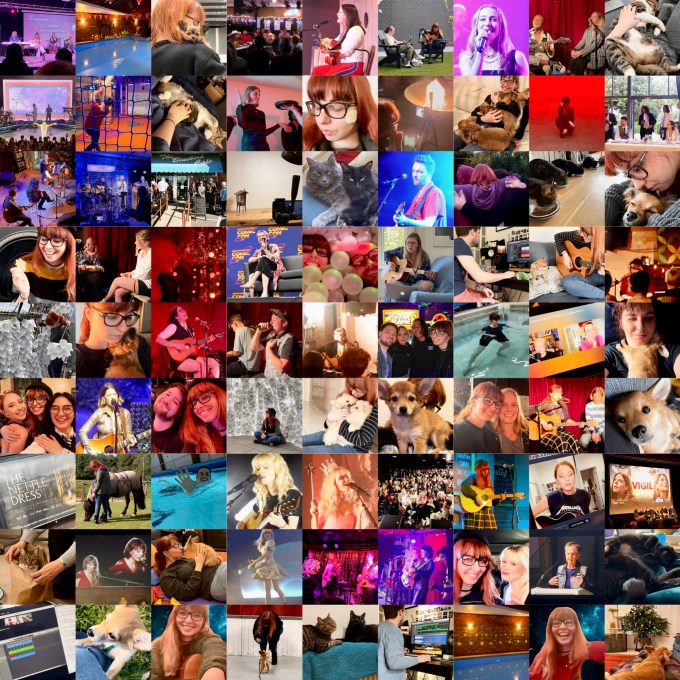
I went to multiple small shows; I went to hydrotherapy religiously and started physiotherapy; I got adopted by a puppy and then had my heart broken when she was taken away; I went to Nashville for Tin Pan South; my application for an Autism Service Dog was successful; I released my single, ‘House on Fire,’ as well as creating all of the visuals for it; I was diagnosed with Fibromyalgia; I went to art exhibitions (and even helped to build my favourite art piece, Breathing Room); I hung out with friends, online and in real life; I travelled to Germany for the wedding of one of my best friends and was reunited with multiple friends that I hadn’t seen in years; I got to hang out with some of my American friends when they performed here; I fought for Taylor Swift tickets; I had my heart broken again when the rescue puppy we applied for was homed with someone else; I went to some amazing concerts; I met Amanda Tapping again and she’s still one of the most wonderful people I’ve ever known; I started performing again; I read books and watched movies and TV shows that are now among my favourites; I adopted a puppy (which still doesn’t sound real to me); I swam 5km for Mind, raising over £600; I went to multiple Maisie Peters shows and got to meet her too; one of my cats got very sick and we had to nurse her back to health; my aunt died; I changed heart medications; and I worked on lots of different musical and academic work. I know all of these things happened; I remember them clearly but it’s like watching them play on a screen. I know these memories are mine but they don’t feel like mine. It’s weird and sad.
I’m so tired. I’m tired of masking but I don’t know how to stop. I feel broken – physically, mentally, and emotionally – but as hard as I try, it never feels like enough. Over ten years later, it should be getting better not worse, right?
I don’t know what else to say. Life feels increasingly scary, internally and externally, and I just feel too broken to manage. I don’t know how people walk around without all of the fear and grief and anxiety that I do, that I see as such an intrinsic part of being human. As I wrote last year, “I don’t know what tomorrow brings. I don’t know what I want it to. I didn’t want this year. I didn’t expect to still be here and I’m not happy or pleased or grateful for that. I feel pathetic and stupid and cowardly; I feel broken beyond repair. I feel frozen, overwhelmed by all of these big feelings. If feelings could kill you, I think these would have.“
Category: animals, anxiety, autism, chronic fatigue, chronic pain, death, depression, diagnosis, emotions, event, family, favourites, heds, hydrotherapy, medication, mental health, pots, self harm, suicide, therapy, treatment Tagged: 2023, actuallyautistic, amanda tapping, antidepressants, asd, autism, autism spectrum disorder, autistic, autistic burnout, autistic singersongwriter, charity, dbt, depression, dialectical behaviour therapy, ehlers danlos syndrome, family, fibromyalgia, heds, hydrotherapy, hypermobile ehlers danlos syndrome, maisie peters, maois, medication, mental health, mental illness, monoamine oxidase inhibitors, new year, new years eve, phenelzine, physiotherapy, radically open dialectical behaviour therapy, rodbt, self esteem, self harm, self injury, self loathing, singersongwriter, songwriter, suicidal ideation, suicidal thoughts, taylor swift, therapy, treatment resistant depression, trigger, trigger warning, year in review
Changing Therapist
Posted on November 5, 2023
TW: Mentions of self harm and suicidal thoughts and urges.
It’s been a year since I started therapy again after an unintentional break, essentially starting again with a new therapist. It’s been a hard and emotional process, and at times a distressing one; just going to therapy can make you feel so vulnerable and so open to further hurt as you dig into the hard stuff – wading into dark waters that you’d rather ignore and pretend don’t exist, even as they’re eroding your mental health – that adding difficulties to that already difficult thing can feel unfairly cruel. So, given that I’m me, I thought that, perhaps, writing about it might be helpful and maybe not just for me but for anyone going through a similar transition. And if not helpful, then hopefully validating in some way.
I’d been seeing Therapist A for almost seven years when everything changed. She was taking leave and I was on my own.
Pre-2021, I’d seen Therapist A once or twice a week pretty consistently since early 2016. Even when the UK went into lockdown due to COVID-19 at the beginning of 2020, we continued our sessions online; I didn’t find them as productive but it was better than nothing. We continued that way for a while, trying to manage my crippling anxiety over the pandemic, working on issues that came up as I persisted with my now online Masters classes, and continuing to work on the issues that had landed me in therapy in the first place. But then the schedule began to slip: Therapist A’s home life was pulling her away from work and I was working myself into the ground in order to complete the final project of my Masters. I barely saw her in the last four months of the course, which I really struggled with: I was digging into some pretty hard stuff, writing song after song about my experience of being autistic, and I craved that safe space to play them to her, to hear her perspective on what I was saying, talk about the feelings they were bringing up, and she wasn’t there. I told myself that it was a short term thing and that, once the Masters was over and her stuff was resolved, the schedule of our sessions would go back to normal. I think it’s safe to say that, given the title of this post, it didn’t.
I finished the Masters in September 2021 and officially graduated, walking the stage, a few months later in November. I had reduced and stopped taking Phenelzine at this point, in preparation for trying ADHD meds (and we all know how appallingly that went), and my depression was creeping back in; the situation was getting pretty desperate. But luckily, that was when Therapist A reached out and we started having sessions again. We had a lot of catching up to do but, by mid-December, we were up to date. Unfortunately, the ADHD medication was already hitting me hard and my depression had gone from a state I recognised to a whole new level of despair with increasingly overwhelming suicidal thoughts. My most vivid memory from that time is sitting in Therapist A’s new office, staring at the unfamiliar rug and hearing my voice in my ears as I confessed to those thoughts, my voice completely flat (this is known as ‘flat affect,’ a recognised symptom of depression and other mental health conditions). It still makes me nauseous to think about, even though so much time has passed and my depression has gotten so much worse since; I think, in my head, that was the beginning of this awful, awful time.
My last session was on New Years Eve and I was drowning, all of the impending new beginnings feeling more like a threat than a promise. When we hung up, I felt achingly hollow and that was only the beginning of a terrible night. But that’s a story for another time. January was passing around me, aimless and anxious, when I finally heard from Therapist A. But instead of setting up our next session, she was letting me know that she was taking leave indefinitely. Her reasons aren’t mine to tell but, between those, my ongoing abandonment issues, and my overwhelmingly bad mental health, I was devastated, spiralling into some grotesque hybrid of a meltdown and a panic attack that went on for hours: I screamed, I cried, I scratched at my face, I tore at my hair, I shrieked like an animal in pain. I guess that’s what I was. I felt like I was trying to exorcise a corrosive demon from my body but nothing helped, nothing alleviated the pain. I was shattered as brutally as if I’d been hit by a wrecking ball. That’s what it felt like, what my life felt like.
Eventually I physically ran out of energy and fell asleep, too tired and emotionally drained to even engage with the world. My depression became more and more overwhelming, compounded by the devastating effects of the ADHD medications and the loss of a massive source of support in my life, and, for months afterwards, I barely got out of bed, barely ate, barely talked. I abandoned social media and I avoided mirrors at every opportunity, to the point where I started to forget what I looked like. The suicidal thoughts were only getting stronger, stronger than they’d ever been in my life, and the feeling of being intrinsically, irreparably broken was – and is – a constant weight in my chest.
I’m not sure when or why I started getting out of bed, why I decided that I needed to go back to therapy. I think I knew I was getting into a very precarious position mentally and the excruciating pain of being inside my head was getting so unbearable that I was willing to do anything to lessen the pressure. I did see a consultant at the local mental health unit but the experience was another traumatic one: after a panic attack at the front door, a junior doctor took my history and then brought in the consultant who told me about ECT and the Ketamine trials before telling me why I shouldn’t do them and recommending doing more of the things I love (which I’d already told him I couldn’t engage with because I was so depressed). So that didn’t improve my relationship with doctors and the medical profession.
For a short while, I worked with a therapist I’d met several years previously but the sessions only made me feel worse and while I have no doubt that it wasn’t intentional, I ended up feeling more broken and more traumatised by some of the things he said, trauma that I’m still carrying around with me. So I stopped seeing him and met with several new therapists, trying to get a feel for them and their methods before committing to someone new. But, just like with Therapist A, Therapist B was the first of the group that I met (a year ago yesterday, I believe) and between her therapeutic approach, her personality, and the fact that she’d brought along a dog she knew in order to put me at ease, she was the obvious choice.
As therapists, they both trained in several of the same disciplines and their skillsets overlap to a certain degree but, when discussing a particular issue, there were differences to how they’d approach it; there has been a fair amount of whiplash in getting use to Therapist B’s approach after so many years with Therapist A. But the point of this post isn’t to compare them – they’re both lovely people and very good at what they do, at least as far as I can tell – but rather to reflect on the process of moving from one to another and the feelings that that kicked up. And a lot of feelings there were – I even wrote a song about it called ‘Grave Digger.’ During the early sessions with Therapist B, we made a timeline of my life and discussed some of the biggest moments, many of which were difficult and distressing (and remain so to this day). Revisiting and recounting the hardest parts of my life was gruelling but I did my best to push through the internal resistance and breathe through the resulting turmoil; between that and the ongoing mental anguish, it was a difficult few months. I don’t mean to make it sound like one continuous torture because that isn’t true -we’ve talked about the good experiences that’ve made me who I am, of course, and there have been sessions where we’ve laughed a lot – but I think that building a strong relationship with a therapist and making progress will always involve periods of incredible vulnerability, which is always scary and, at times, painful.
Sometimes – okay, often – I feel like I’m not making any progress at all, partly because of all the disruption and the distress it’s caused. A year ago, I hadn’t expected to see 2023 and my depression and chronic suicidal thoughts haven’t lessened, even though I am taking Phenelzine again (at a higher dose, in fact) – after many discussions with Therapist B. It has made me more functional, to a certain degree, but the decision came with a price tag: my self harming escalated from cutting my arm to cutting my face. I’m not convinced anything’s changed; I don’t feel any better. But I can see that some things have changed and changed for the better, even though I can’t feel the effects yet: something has allowed me to start talking about some of the worst stuff in my brain, even if only a little. It’s something I could never have imagined doing so I know that that’s progress, even though I struggle to feel it.
I have heard from Therapist A several times now; the news has generally been positive, which has been a great relief (and I appreciate having a little less uncertainty in my life). Therapy is continuing as normal – the current version of normal at least – which I’m pretty sure is a good thing: the idea of trying to work my way through all of the emotions that I know would come up as a result of any potential change makes me feel physically nauseous.
I’m not always convinced that I’ve adjusted and sometimes I forget that I’m not going to see Therapist A, my body moving in the direction of that office as the car turns down a different road; that experience is more ingrained than I had realised at the time. And I know I’m still carrying a lot of hurt and anger over the whole thing, even though over a year has passed. I’m not angry at the people involved – nobody chose any of this – but there is anger and, although I’ve been slower to realise it, hurt too. I think it’s easier to be angry than to be hurt. Not always but sometimes. And, as I said, I have abandonment issues, issues that I’ve struggled with for a long time, which – unsurprisingly – have been exacerbated by this whole thing. It’s hard to lose someone that you trusted to never leave (a naïve ideal, I know) and it’s hard to trust someone new, ignoring the whispers that they’re just another person who will inevitably walk away. I think these issues are important to mention but they probably need their own blog post rather than taking up space here: when talking about changing therapists, it’s not something that everyone has mixed into the equation. All of that said, I’m trying to trust and I think that, for the most part, I am, even if it does sometimes feel like a conscious, concentrated effort. The progress isn’t as fast as I’d hoped it would be when I committed to therapy again last year but the proof is there. I’m sharing things I never thought I’d share and that’s certainly not nothing.
Category: about me, anxiety, autism, covid-19 pandemic, depression, emotions, medication, meltdowns, mental health, self harm, suicide, therapy, treatment, university, writing Tagged: abandonment, abandonment issues, actuallyautistic, adhd, adhd medication, antidepressants, asc, asd, attention deficit hyperactivity disorder, autism, autism spectrum condition, autism spectrum disorder, autistic, autistic adult, autistic artist, autistic meltdown, autistic songwriter, covid, covid-19, cptsd, dbt, depression, dialectical behaviour therapy, ect, electroconvulsive therapy, fear of abandonment, flat affect, graduation, ketamine, ketamine trials, masters, masters degree, masters degree in songwriting, medical trauma, medication, meltdown, mental illness, online therapy, panic attack, phenelzine, radically open dialectical behaviour therapy, rodbt, self harm, self injury, songwriter, songwriting, suicidal, suicidal ideation, suicidal thoughts, suicidal urges, therapist, therapy, trauma, trd, treatment resistant depression, university
World Mental Health Day 2021
Posted on October 10, 2021
‘MENTAL HEALTH IN AN UNEQUAL WORLD’
As I’m sure many of you know, today is World Mental Health Day and the theme, chosen by the Mental Health Foundation, is ‘mental health in an unequal world.’ WHO seems to be building it around the pandemic, rather than as a problem of its own, but from what I’ve seen in the newsletters and on the social medias of many mental health charities and organisations, most seem to be following the lead of the Mental Health Foundation.
According to the Mental Health Foundation’s website: “2020 highlighted inequalities due to race and ethnicity, sexual orientation and gender identity, and the lack of respect for human rights in many countries, including for people living with mental health conditions. Such inequalities have an impact on people’s mental health. This theme, chosen for 2021, will highlight that access to mental health services remains unequal, with between 75% to 95% of people with mental disorders in low and middle-income countries unable to access mental health services at all, and access in high income countries is not much better.” It goes on to say: “Many people with a mental illness do not receive the treatment that they are entitled to and deserve and together with their families and carers continue to experience stigma and discrimination… The stigma and discrimination experienced by people who experience mental ill health not only affects that person’s physical and mental health, stigma also affects their educational opportunities, current and future earning and job prospects, and also affects their families and loved ones.”
Statistics provided by Mind (x)
I have my own experience with the mental health system – which I do want to touch on – and have heard from many others about their experiences but I wanted to read into the research around these inequalities further, both to get a better factual understanding and to put my own experience in context (beyond an anecdotal one). The research is sporadic at best but here are some of the statistics I found…
ACCESS TO MENTAL HEALTH CARE
- “NICE [The National Institute for Health and Care Excellence] recommends that people should be able to access services when they need them. However the proportion of people who felt they had definitely seen NHS mental health services enough for their needs reduced from 47% in 2014 to 43% in 2018.” (x)
- In 2020, it was reported that approximately 1 in 3 people who experience mental health problems are able to access the support they need. (x)
From these statistics, it’s clear that far too many people aren’t getting the support that they need.
INEQUALITIES IN ACCESS TO TREATMENT (x)
- For those with common mental health problems, 36.2% reported receiving treatment.
- Women are more likely than men to receive treatment for all mental health conditions, with 15% of women receiving treatment compared to 9% of men.
- Young people aged 16-24 were found to be less likely to receive mental health treatment than any other age group.
- White British people are more likely to receive mental health treatment (13.3%) compared to BAME groups (7%). The lowest percentage of people receiving treatment were those from black ethnic minority groups (6.2%).
These statistics clearly show the disparities in the availability of treatment, more supporting evidence for the statement that the Mental Health Foundation is making with the theme for this World Mental Health Day.
YOUNG PEOPLE
- “There is very little national information about mental health services for children and young people, and what information there is suggests quality is declining. [Research] indicates substantial cuts to services, increasing demand, increasing thresholds for treatment, very long waits (more than a year) for specialist services, and a resultant decline in accessibility.” (x)
- Approximately 1 in 3 children and young people with a diagnosable mental health condition get access to NHS care and treatment. (x)
- More than 338,000 children were referred to CAMHS in 2017, but less than a third received treatment within the year. (x)
- Around 75% of young people experiencing a mental health problem are forced to wait so long their condition gets worse or are unable to access any treatment at all. (x)
- In a YoungMinds survey, three-quarters (76%) of parents said that their child’s mental health had deteriorated while waiting for support from Child and Adolescent Mental Health Services (CAMHS). (x)
This research all indicates that young people in particular are being let down by the health care system.
SECONDARY [LONG TERM] CARE
- “Demand for secondary care (which generally treats people with severe mental health problems) is increasing, and there is evidence to suggest services are becoming less accessible… There is little information available on the outcomes that services achieve.” (x)
- “There is no high quality national information on waiting times for secondary mental health services. In a 2014 survey, 20% of people with severe mental illness who were offered talking therapy reported waiting more than a year to access it.” (x)
The statistics show not just that the need for mental health care is increasing but the need for long term mental health care is increasing but that it’s also very difficult to access.
HIDDEN WAITING LISTS (x)
“A study of 513 British adults diagnosed with a mental illness also reveals the damaging consequences that hidden waiting lists – the wait between referral and second appointments – have on the lives of patients living with severe or common mental illness.”
- “Of those on a hidden waiting list, nearly two thirds (64%) wait more than four weeks between their initial assessment and second appointment. One in four (23%) wait more than three months and one in nine (11%) wait longer than six months.”
- “Respondents living with severe mental illness – including eating disorders, bipolar disorder and PTSD – were left waiting up to two years for treatment. Others were left waiting up to four years for treatment for depression, anxiety and suicidal thoughts.”
- “Two-fifths (38%) reported that they, or someone on their behalf, had contacted emergency or crisis services while waiting for their second appointment, while 39% said that waiting led to a decline in their mental health.”
It’s clear that, beyond the difficulty of even getting into the mental health care system, once in it, the process of actually getting the support you need is much too slow – so slow in fact that it’s exacerbating the mental health problems that those waiting are seeking help for.
Now I want to look at my experience of getting support for my mental health…
- For more than two years, I was repeatedly dismissed and had my feelings and experiences invalidated by multiple doctors and services. No one took me seriously. Eventually, my Mum took me to a private psychiatrist and I was diagnosed with Generalized Anxiety Disorder, Social Anxiety Disorder, Depression, and OCD. Having had no idea what I was struggling with, I’d done a lot of research and asked about the quiet presentation of Borderline Personality Disorder, which my psychiatrist initially rejected but then reconsidered and diagnosed me with it after reading my research and personal notes (it has since been recommended to me multiple times – sometimes by doctors who don’t even know me – that I have this diagnosis removed from my file because “people might make assumptions”). Getting an NHS referral for an Autism Diagnostic Assessment was similarly difficult as he felt that I didn’t fit the classic presentation (I do apparently fit the classic FEMALE presentation though).
- There was no follow up after this diagnosis and we were told there was no support available so my Mum investigated private therapists. I tried CBT for a while but didn’t find it helpful so I tried DBT instead, which has been a much better fit.
- All of this private treatment is obviously not cheap and I am so beyond grateful that my family is fortunate enough to support me financially. I honestly don’t know where I’d be without it, whether I’d even be here. But the cost of it does cause me significant worry, only adding to the anxiety I already experience.
- With so many of my problems connected to my Autism, had this whole process been… easier, simpler, quicker, less traumatic, or something… so many of my health problems wouldn’t have deteriorated to the level that they have. Had I been diagnosed earlier – had even one medical professional believed me – things might’ve been so different. I try not to dwell on that because there’s no point wasting my energy on what might have been but it is the truth.
- Having said that, considering some of the stories that I’ve read or have had shared with me, my story isn’t that bad. I’m positively lucky compared to some and that’s a confusing, complicated thing to say, knowing how traumatic this has all been… and continues to be.
Since then, I’ve developed near constant chronic pain throughout my body – something that’s obviously had a big impact on my mental health – but over a year later, I’m still waiting for the NHS physiotherapy and hydrotherapy referrals to go through. I have started Occupational Therapy and with the Pain Clinic (both through the NHS) but with the end of my Masters, I had to take a break because they were too painful and/or upsetting to manage alongside all the work. I’m starting back this week. It still bothers me that no one’s ever even tried to find out why the pain started though.
Almost six years after my ASD diagnosis, the Neurobehavioural Clinic called to offer me an appointment, to do what I had no idea. But at the end of the two part session, I’d been diagnosed with Hypermobile Ehlers-Danlos Syndrome and ADHD – aged twenty six – both conditions having gone unnoticed because no one had ever taken my associated problems (problems that have been there my whole life) seriously. They’re both conditions that often occur alongside ASD. The hEDS diagnosis would, in theory, push my physiotherapy and hydrotherapy referrals but, as I said, I haven’t heard anything and almost a year later, my ADHD is still untreated. My psychiatrist was happy to ‘move’ that condition to his care but the consultant I saw didn’t want that, which is especially frustrating because she’s so difficult to get in contact with.
And finally, I may be getting answers to another ongoing medical problem: severe dizziness, light-headedness, nausea, physical weakness, and breathlessness when I stand up for too long. We’ve been trying to get support around this for so long that I can’t even remember when it started. This too may well be related to my Autism and I can’t help thinking that it’s another thing that should’ve been discovered sooner.
All of these things have had a profound impact on my mental health and going through the agonising process of diagnosis again and again has left me wary, fearful, and angry at medical professionals. It’s deeply ingrained in me to be polite and respectful but it doesn’t take much to send me flying off the handle; I walk into each appointment feeling like a tightly coiled spring. I leave pretty much every appointment in tears at best, raging at worst. Because I’m so. freaking. tired. of feeling like this. Of feeling like no one believes me, of being made to feel like I don’t know what I’m talking about, of being made to feel like I don’t know what I’m feeling. I feel so worn down by the constant let downs. At this point, I think I’m only going back because I don’t know what else to do.
I have no doubt that social media will be filled with nice words and encouraging quotes today. But we need more than that. World Mental Health Day is about more than that. Or it should be. It should be about pushing for change and improvement. The Mental Health Foundation is absolutely right that the inequalities in the mental health care system need to be addressed but looking at these statistics, it’s also clear that the standard of care needs to be better. For everyone’s sake. After all, there’s very little difference between not getting any support and being on a list waiting years for support.
Category: about me, adhd, anxiety, autism, bpd, depression, diagnosis, emotions, heds, medication, mental health, ocd, research, therapy, treatment Tagged: accessibility, adhd, asd, attention deficit hyperactivity disorder, autism, autism spectrum disorder, borderline personality disorder, bpd, camhs, cbt, chronic pain, dbt, depression, diagnosis, diagnostic process, eds, ehlers danlos syndrome, gad, generalized anxiety disorder, heds, hypermobile ehlers danlos syndrome, medical trauma, medication, mental health, mental health awareness, mental health care, mental health foundation, mental health in an unequal world, mental health in the media, mental health services, mental health stigma, mental health treatment, mental illness, mental illness awareness, mental illness stigma, neurodiversity, nhs, obsessive compulsive disorder, ocd, private health care, private mental health care, private psychiatric care, research, social anxiety, social media, statistics, stigma, therapy, wmhd, world mental health day, world mental health day 2021

About Me
Hi! I’m Lauren Alex Hooper. Welcome to my little blog! I write about living with Autism Spectrum Disorder (ASD), ADHD (Inattentive Type), and Hypermobile Ehlers-Danlos Syndrome (hEDS), as well as several mental health issues.
I’m a singer-songwriter (it’s my biggest special interest and I have both a BA and MA in songwriting) so I’ll probably write a bit about that too.
My first single, ‘Invisible,’ is on all platforms, with all proceeds going to Young Minds.
My debut EP, Honest, is available on all platforms, with a limited physical run at Resident Music in Brighton.
I’m currently working on an album about my experiences as an autistic woman.
Links
Categories
Recent Posts
Archives
- January 2026 (1)
- December 2025 (1)
- August 2025 (1)
- July 2025 (1)
- June 2025 (4)
- May 2025 (3)
- April 2025 (2)
- March 2025 (1)
- February 2025 (1)
- January 2025 (1)
- December 2024 (2)
- November 2024 (1)
- October 2024 (1)
- July 2024 (1)
- May 2024 (1)
- April 2024 (3)
- March 2024 (1)
- January 2024 (1)
- December 2023 (4)
- November 2023 (6)
- October 2023 (5)
- September 2023 (6)
- August 2023 (4)
- July 2023 (5)
- June 2023 (5)
- May 2023 (7)
- April 2023 (4)
- December 2022 (4)
- November 2022 (1)
- October 2022 (1)
- September 2022 (1)
- August 2022 (3)
- June 2022 (2)
- May 2022 (6)
- April 2022 (10)
- March 2022 (9)
- February 2022 (3)
- January 2022 (1)
- December 2021 (7)
- November 2021 (5)
- October 2021 (7)
- September 2021 (4)
- August 2021 (1)
- July 2021 (2)
- June 2021 (4)
- May 2021 (10)
- April 2021 (11)
- March 2021 (14)
- February 2021 (6)
- January 2021 (6)
- December 2020 (8)
- November 2020 (9)
- October 2020 (8)
- September 2020 (10)
- August 2020 (8)
- July 2020 (4)
- June 2020 (6)
- May 2020 (8)
- April 2020 (7)
- March 2020 (9)
- February 2020 (5)
- January 2020 (7)
- December 2019 (7)
- November 2019 (1)
- October 2019 (1)
- August 2019 (1)
- July 2019 (2)
- June 2019 (3)
- May 2019 (5)
- April 2019 (5)
- March 2019 (5)
- February 2019 (6)
- January 2019 (5)
- December 2018 (7)
- November 2018 (3)
- October 2018 (5)
- September 2018 (5)
- August 2018 (5)
- July 2018 (9)
- June 2018 (7)
- May 2018 (7)
- April 2018 (6)
- March 2018 (11)
- February 2018 (5)
- January 2018 (6)
- December 2017 (7)
- November 2017 (7)
- October 2017 (7)
- September 2017 (6)
- August 2017 (5)
About Me
Hi! I’m Lauren Alex Hooper. Welcome to my little blog! I write about living with Autism Spectrum Disorder (ASD), ADHD (Inattentive Type), and Hypermobile Ehlers-Danlos Syndrome (hEDS), as well as several mental health issues.
I’m a singer-songwriter (it’s my biggest special interest and I have both a BA and MA in songwriting) so I’ll probably write a bit about that too.
My first single, ‘Invisible,’ is on all platforms, with all proceeds going to Young Minds.
My debut EP, Honest, is available on all platforms, with a limited physical run at Resident Music in Brighton.
I’m currently working on an album about my experiences as an autistic woman.
 Finding Hope
Finding Hope

