Fully Vaccinated!
Posted on June 19, 2021
Since I’m in a one of the vulnerable groups, I have now had both of my Covid-19 vaccines! Yippee!
Back at the end of March, I had my first vaccine. I’ve had so many blood tests and procedures involving needles that the vaccine itself really didn’t phase me, not that I’m exactly a fan of being poked by pointing things. I was a bit nervous about what the side effects might be but being vaccinated was worth it, I had no doubt. The staff at the vaccination centre were kind and efficient; I was in and out in less than twenty minutes.
The only side effect I’m sure was connected to the vaccine was how tender my arm was afterwards. After the first vaccine, it was so sore that I could barely touch the injection site for two weeks. I slept terribly because I woke up every time I rolled onto that side and that arm. After two weeks, it finally disappeared.
I had several migraines in the month after, the first of which resulted in a trip to A&E to make sure I didn’t have the rare Astra Zeneca side effect of blood clots. I didn’t and it was just a migraine but then I had several more, much higher than my monthly average. I couldn’t and still can’t be sure that they were caused by the vaccine – due to the abscess in one of my teeth that was later diagnosed, which could’ve also been causing them – but I’ve never had that many migraines in such a short period of time.
Even having the one vaccine made me feel better, safer. I obviously didn’t stop wearing a mask or social distancing, but I just felt like I had that extra layer of protection. It made my anxiety (and sometimes panic) about going out just that bit smaller.
Middle of June and I got the text to go back for my second dose. I managed to book a slot within the week, which I was already impressed with, but then it was brought forward. Doubly impressed. Everyone at the vaccination centre was super efficient and really nice and again, I was in and out in less than twenty minutes. Again, I had the tenderness in my arm but it didn’t last nearly as long; it was gone within a few days. I did have a migraine a few days after but it only last for a day rather than the almost week long migraines I was suffering from before (although, as I said, it’s hard to determine what caused those with the tooth problem). And fingers crossed, that will be the only one. I had heard that people generally experienced fewer side effects after their second vaccine but I hadn’t wanted to put too much stock in it just in case I didn’t have the same experience; I didn’t want to set myself up to be disappointed or frustrated. But, almost a week on from the second dose, everything seems to be okay and within a couple of weeks, I will officially be fully vaccinated and as protected as I can be at this moment in time and that is a big relief.
Living With Unmedicated ADHD
Posted on June 12, 2021
It’s been a while since I last talked about my ADHD so I thought it was time for a little update. A lot has happened since I was diagnosed, some of which I thought might be worth sharing…
It was a lot to process that I did my BA and have been doing my MA with undiagnosed and unmanaged ADHD but the diagnosis had me looking back over the last few years and a lot of things started to make sense: why I’d excelled in certain areas and struggled desperately in others. Part of me was impressed with how I’d done, factoring in this new obstacle that I’d been unknowingly battling against, but on the other hand, it makes me sad that I’ve had to, you know? It makes me sad that I’ve had to work against my own mind all this time without anyone noticing or supporting me – in this sense, at least. Life could’ve been so much easier.
And now I have to finish my Masters unmedicated.
Because I take Phenelzine for my depression, there’s the risk of interactions with stimulant-based ADHD medication so I can’t take those; both medications have the potential to raise a person’s blood pressure and together, that could be very dangerous. However, given the extreme drowsiness I experience as a side effect of the Phenelzine, I can’t take a non-stimulant medication either due to the high chance that they’ll add to the drowsiness. It’s hard enough staying awake and (somewhat) focussed during the day. I can’t afford to make it worse, especially in this final module of my Masters, the one I’ve been looking forward to since I started the Masters. So it looked like a dead end. But I wasn’t giving up at the first hurdle so I did what I always do: I started researching.
After a bit of searching, I found a research paper about a series of studies done, combining medications when traditional routes failed to work. One of those cases detailed a man who only responded to an MAOI (which is what Phenelzine is) and a stimulant-based ADHD medication. He had to continuously monitor his blood pressure but had no problems and continued on the two medications indefinitely, which allowed him to live a normal, productive life. That seemed very promising, as a starting point for discussion at the very least, so I sent it to both my psychiatrist (who’s been managing my medication for years now) and the ADHD specialist.
My psychiatrist was willing to try, provided I was diligent about checking my blood pressure. Despite our initial ups and downs, we have a really good relationship – and we have had for a long time now – and he always takes my thoughts, opinions, and research into consideration, which I really appreciate even if he ultimately opts for a different approach. So that felt good, like a step in what felt like a positive direction.
We didn’t get a response from the ADHD specialist for weeks. To begin with it was just frustrating but as time went on, I started to swing between despair and anger. I felt like I’d just been abandoned, dropped without a word (something that’s unfortunately happened enough times that it’s become a big trigger for anxiety attacks, episodes of depression, and even autistic meltdowns, depending on the situation); sometimes it feels so upsetting that these medical professionals can just go home at the end of the day and leave all of the struggles of their patients/clients behind while we all have to keep living (and suffering) from them. I know it’s not that simple – that they don’t just stop caring, that they can’t and shouldn’t have to work ridiculous hours – but in my desperate moments, in situations like this, it feels hard to feel supported, to believe that they do care, that you’re not just another file rather than a person struggling through each hour.
After some extra complications due to communication problems, we finally heard back and she was saying a categorical no, having had previous patients respond badly to the combination. While I can understand that, I found it frustrating that she wasn’t even open to trying it. I’ve always responded unusually to medications (proven again and again by my experiences with more than fifteen medications/combinations for my depression – the only one that’s worked is one that’s rarely used) so I was frustrated by the brick wall approach she was taking. My psychiatrist was still open to trying and said he’d talked to her about transferring the medication aspect of managing my ADHD to him since he’s been treating me for so long and has a detailed understanding of my history. But she said no.
So that’s it as far as I can tell. Unless I change my antidepressant, (I have to point out again) the only one that’s helped me, I can’t take medication for my ADHD. It’s essentially come down to choosing which of the conditions to treat, my depression or my ADHD, which just makes me feel so upset and frustrated. Treating my ADHD could make a huge difference in finishing my Masters but I’m getting blocked at every turn. It’s almost worst now than before I knew about the ADHD. Before, I was struggling; now, I’m struggling and I know why but I can’t do anything about it. The whole situation makes me so angry, so angry that I couldn’t do the most recent online appointment. I wasn’t in the right headspace and I doubted my ability to be receptive when my emotions were so all over the place.
My Mum took the meeting but it hasn’t changed anything. I’m still not getting any treatment, any support. I feel like I’ve been given this great weight to carry but abandoned to carry it without help or advice. I don’t know what to do. I don’t know how to move forward. I feel like I’ve been let down by someone who’s job it was to help me. Again. It’s upsetting and exhausting and stressful.
I don’t say these things to encourage a mistrust of doctors or because I regret the ADHD diagnosis. I just need to be honest – for the sake of my own mental health – and while I generally try to see the positive, sometimes the situation just sucks. It’s just bad and hard and makes a mess of you.
Migraines, Tooth Pain, And Blood Pressure Monitoring
Posted on June 5, 2021
So often in my life it seems, medical stuff is like waiting for a bus: weeks or months go by and then suddenly a whole slew of them show up. And that’s certainly been true of the last few months. Just as the final module of my Masters was starting, I was hit by a series of awful migraines, suffered with terrible tooth pain, and spent twenty four hours hooked up to a blood pressure monitor, a test ordered by a neurology unit in London. So it’s been a pretty hectic time…
MIGRAINES
At the time of writing this, I’ve lost approximately half of the last forty days to migraines.
I’ve had migraines before – maybe a handful a year, depending on my stress levels and the medication I’m taking – but they usually only last for a day or so before fading away. They’re not pleasant but they weren’t seriously impacting my life. But then I had one that lasted roughly four days and I ended up in A&E because, having fairly recently had the Astra Zeneca vaccine, my doctor was worried about the extremely rare side effect of a blood clot. I was sure it was a migraine but agreed to go and after most of the day there, I was released; the doctor agreed that it was most likely a bad migraine but told me to come back if it didn’t go away. And after another day or so, it did. While I was somewhat irritated about losing a day that should’ve been spent working on my end of semester assessment (despite the pain, I was pushing myself to work on it as I could, in the moments where the painkillers actually worked – I think that’s mainly why it went on so long personally), I am really grateful to all of the hospital staff. They were all great – warm, considerate, and personable – despite the somewhat alarming COVID precautions everywhere that weren’t exactly great for my anxiety. But they were really kind and gentle with me throughout my visit, making the whole experience a lot easier than it could’ve been.
I’d thought that that was it. But then, again and again, I was hit by migraine after migraine, all lasting unusually long periods of time (for me, at least). They were averaging out at about six days each time, sometimes more. That was extremely stressful, bearing in mind that I’m at the beginning of the homestretch of my Masters with this final module accounting for 60% of my final grade, and I was utterly miserable from the pain. I was also so light sensitive; at one point, even the darkest room in the house felt too bright and I dissolved onto the floor in tears, which only hurt my head more. It was awful. That was the first time we called 111 and they called paramedics. That time they determined it was, again, a severe migraine and recommended two other pain medications to try in the hope that they’d be more effective than Nurofen.
A couple of migraines later, with minimal help from the new painkillers, I had another really bad one, which had us calling 111 and they sent paramedics (both such lovely guys who fell in love with the cats and talked musicals with me while they did their tests). This migraine was slightly different: it had all of my normal migraine symptoms but I also had this almost blinding pain at the front and right side of my face. They thought it was probably a migraine but suggested talking to my doctor about having a CAT scan and/or whether there was something going on with my cranial nerves. They also had some practical, experience based advice around pain relief (one of them had personal experience with severe migraines). They said they could escort us to the hospital on the off chance that a doctor would do a CAT scan but did acknowledge that they might just take blood and keep me there while it was checked again, like my previous visit to A&E. So we chose the second option: Mum was going to go out and get the new medication option and call my GP ASAP.
TOOTH PAIN
That was the most recent migraine (at the time of writing this). As time passed, the pain in my head started to decrease, then my face, settling in my back-top-right teeth; every time they – and finally just one (after about a week) – knocked against the bottom teeth, the pain was so bad that my entire body would freeze up.
As soon as it had settled in my teeth, we’d called the dentist and they brought me in as an emergency (a few days wait rather than a few months). The dentist checked, took x-rays and saw some decay in the painful tooth, fairly close to the nerve root, and it already has a pretty big filling in it. At one point, somehow, the hEDS diagnosis came up (I was diagnosed since my last dental appointment) and the dentist said that she’s seen and heard about multiple people with a form of EDS (or who were later diagnosed with it) struggle with tooth decay, as well as being scolded by their dentists for not doing a good enough job with their dental hygiene even though they actually were; it was often the EDS causing problems, not necessarily their actions. This really is the diagnosis that keeps on giving (imagine a sarcastic snort at the end of that sentence).
Anyway, she diagnosed an abscess and gave me two treatment options: extraction or root canal therapy, which would involve multiple, multi-hour sessions that would be painful, ultimately might not work, and probably wouldn’t last into my late thirties. The whole thing felt pretty overwhelming and I ended up in tears. Extraction was the obvious choice as far as I was concerned and everyone else agreed; there seemed to be way too many downsides to the root canal option (plus it sounded horrendous and I find dental work, even fairly straightforward stuff, very distressing) and even if I was inclined to choose it, it’s the worst possible time given the end of my Masters. Even an extraction is going to be a significant disruption. I’m applying for extenuating circumstances, which both my supervisor and module leader have encouraged, so hopefully that’ll mean I end up with the same amount of time to do the work as everyone else.
So, I’ve been referred for an emergent extraction under general anaesthetic but I don’t know when that’s going to happen. They also prescribed me some antibiotics for the mean time. Now it’s a waiting game. But several days after the appointment, either the antibiotics are working or the nerve is dying or both because the pain is getting better and I feel more human. There are periods of time where I can actually ignore it, which is a huge deal considering how much pain I’d been in. So that’s definitely something to be grateful for.
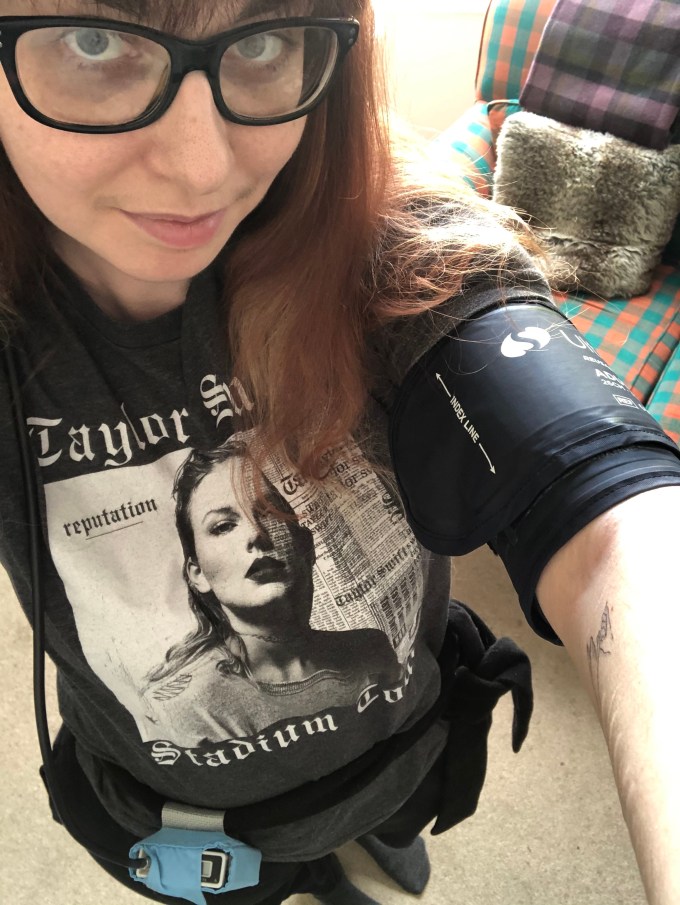
BLOOD PRESSURE MONITORING
A couple of months ago, I had an appointment with a doctor from a neurology unit in London, which I believe I mentioned in this post. After spending most of the appointment vehemently telling me there was no point in getting any tests, he somewhat reluctantly offered to write to my GP, suggesting I have my blood pressure monitored for twenty four hours. It took forever to get a monitor from the hospital but finally test day came.
I had to go to the hospital where they fitted the monitor (found the right size for my arm, wrapped me up, made sure it was taking readings, looped the cable behind my neck, and used the tie from my coat to secure the monitor/data recorder around my waist) and gave me the instructions and paperwork to go along with the monitor. I wasn’t allowed to get it wet so I couldn’t have a shower while wearing it but since that’s when I usually get my blood pressure related symptoms, we devised a plan where I would go through the motions – with the shower on to create the heat and steam – so that it would still record whatever was happening to my blood pressure during a shower, as much as possible at least. The whole process was relatively stress free and the two women who sorted me out were great, warm and extremely competent but flexible to my needs. I’m really grateful to them for making it so easy.
All done, we headed home. It was a bit weird with the weight of the monitor, the too long cable getting caught on stuff, and so on but overall, it was fine. The cuff got very tight – tighter than I remembered them getting when you get a one off test – but it wasn’t a big deal and the rest of the day went on as normal. It was a bit of a struggle to get to sleep because I couldn’t get comfortable with the cuff on my arm but once I did get to sleep, the inflating and squeezing didn’t wake me up, something I’d expected to happen.
However, when I woke up, my arm was really sore. I felt like I’d been punched a hundred times in the same place, convinced the skin was bruised underneath the cuff (it wasn’t and no bruise ever emerged but damn, it was tender). I think the cuff had slipped in the night as well because I had several error readings on that second day.
I had my pretend shower and, as usual, felt shaky, dizzy, and lightheaded; having thought ahead, I’d timed things so that the monitor would be taking the reading right at the end of my fake shower. I’m intrigued to see what that reading says. That done, Mum helped me wash my hair, leant over the side of the bath; I had an online meeting and couldn’t bear the thought of doing that with unwashed hair. It wasn’t very dignified, especially with all the extra towels wrapped around me to keep the monitor dry, but it got the job done.
I wore it for the rest of the twenty four hours and then, with great relief, unwrapped the cuff. By the end, my arm felt really sore from the squeezing, plus it had started to pinch in various places at some point. There’s also that Autism-sensory-thing of wearing something constantly constricting, which starts causing anxiety after certain periods of time, like a long day in skinny jeans or wearing my retainer all day. Does that make sense? The anxiety had been building for the last few hours and it was wonderful to take it off.
Mum dropped it back at the hospital, so now I guess it’s another waiting game. I don’t know when we’ll find out the results and the conclusions drawn from them. I assume that they’ll let us know at some point, although it wouldn’t be the first time we’ve had to chase results. As I said, all we can do now is wait.
So, yeah, hectic. At a very inconvenient time. But that’s life and I’m determined not to let it spoil the last of my Masters and this project that I’ve been looking forward to for so long. I am going to make the most of every good day I have, take the extenuating circumstances gratefully, and continue working as hard as I can.
 Finding Hope
Finding Hope